Transperineal Prostate Biopsy Shown to Have Zero Infection Risk Compared to Transrectal Approach
المفاهيم الأساسية
Transperineal prostate biopsies have a significantly lower infection risk compared to the traditional transrectal approach, with no infections observed in the transperineal group.
الملخص
This article discusses the findings of a multicenter, randomized trial that compared the safety and cancer detection rates of transperineal (TP) and transrectal (TR) prostate biopsies. The key highlights are:
- The study involved 372 patients who received TP biopsies without antibiotics and 370 patients who received TR biopsies with antibiotics over 3 years at 10 centers.
- No infections were observed in the TP group, while 1.6% of the TR group developed infections, mainly urinary tract infections.
- The cancer detection rates were similar between the two groups, with high-grade cancer found in 55% of TP biopsies and 52% of TR biopsies.
- The researchers argue that TP biopsies should become the standard of care, as they enable antibiotic stewardship and have a significantly lower infection risk.
- Current guidelines by the American Urological Association and National Comprehensive Cancer Network give equal standing to TP and TR biopsies, while the European Association of Urologists favors TP biopsies.
- Experts believe that TP biopsies can help detect cancer in areas that the TR approach may miss, and that raising public awareness is key to driving wider adoption of the TP method.
تخصيص الملخص
إعادة الكتابة بالذكاء الاصطناعي
إنشاء الاستشهادات
ترجمة المصدر
إلى لغة أخرى
إنشاء خريطة ذهنية
من محتوى المصدر
زيارة المصدر
www.medscape.com
Is This the Best Prostate Biopsy?
الإحصائيات
No infections were observed in the transperineal biopsy group.
1.6% of the transrectal biopsy group developed infections, mainly urinary tract infections.
High-grade cancer was found in 55% of transperineal biopsies and 52% of transrectal biopsies.
اقتباسات
"Our study shows a very low 0% infection risk, without the need for preventative antibiotics, which can potentially save lives."
"The rate of infections in all of the randomized clinical trials is low and the infections are typically mild; this should allay the public's concerns about prostate biopsy-related infections."
الرؤى الأساسية المستخلصة من
by Howard في www.medscape.com 09-19-2024
https://www.medscape.com/viewarticle/transperineal-biopsies-show-superior-safety-over-transrectal-2024a1000h3c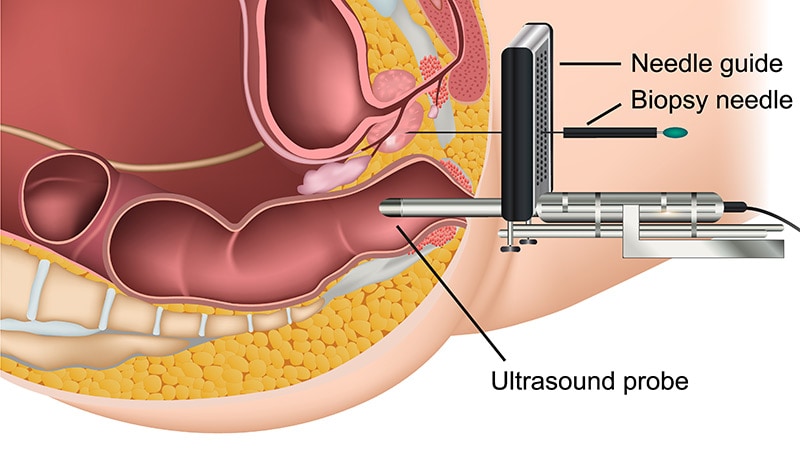
استفسارات أعمق
What are the potential long-term implications of reduced antibiotic use in the transperineal biopsy approach?
The reduced antibiotic use in the transperineal (TP) biopsy approach has several potential long-term implications. Firstly, it promotes antibiotic stewardship, which is crucial in combating the growing global issue of antibiotic resistance. By minimizing the reliance on prophylactic antibiotics, the TP method may help preserve the effectiveness of existing antibiotics for future medical needs. This is particularly important as antibiotic resistance can lead to increased morbidity and mortality from infections that were once easily treatable.
Secondly, the absence of antibiotic pretreatment in TP biopsies may lead to a decrease in the incidence of antibiotic-related side effects, such as gastrointestinal disturbances or allergic reactions, which can affect patient compliance and overall health. Furthermore, the 0% infection rate observed in the TP group suggests that this method may enhance patient safety and satisfaction, potentially leading to higher acceptance rates of prostate biopsies among men who might otherwise avoid the procedure due to fear of complications.
Lastly, the long-term implications may extend to healthcare costs. With fewer infections, there could be a reduction in the need for follow-up treatments, hospitalizations, and additional healthcare resources, ultimately leading to cost savings for both patients and healthcare systems.
How might the cost-effectiveness of the two biopsy methods compare, considering factors like infection rates and cancer detection?
When comparing the cost-effectiveness of transperineal (TP) and transrectal (TR) biopsy methods, several factors must be considered, including infection rates, cancer detection rates, and overall healthcare costs. The TP biopsy method has demonstrated a significant advantage in terms of infection rates, with a 0% infection rate compared to a 1.6% infection rate in the TR group. This difference suggests that TP biopsies could lead to lower costs associated with treating infections, which can include hospital stays, additional medications, and follow-up care.
In terms of cancer detection, both methods showed similar rates of high-grade cancer detection, with TP biopsies identifying 55% and TR biopsies identifying 52%. This parity in cancer detection means that the TP method does not compromise diagnostic accuracy while offering a safer profile.
Moreover, the potential for reduced antibiotic use in TP biopsies can lead to further cost savings, as the need for antibiotic prophylaxis and the associated costs of managing antibiotic resistance are minimized. Overall, while the initial costs of TP biopsies may be comparable to TR biopsies, the long-term savings from reduced infection rates and the avoidance of complications could make TP biopsies more cost-effective in the long run.
What other emerging technologies or techniques could further improve the safety and accuracy of prostate cancer diagnosis in the future?
Several emerging technologies and techniques hold promise for improving the safety and accuracy of prostate cancer diagnosis. One notable advancement is the use of MRI-guided biopsies, which allow for more precise targeting of suspicious lesions identified through imaging. This technique can enhance cancer detection rates while minimizing the risk of complications associated with traditional biopsy methods.
Another promising development is the integration of artificial intelligence (AI) in the analysis of biopsy samples and imaging data. AI algorithms can assist pathologists in identifying cancerous cells more accurately and quickly, potentially leading to earlier diagnosis and treatment. Additionally, AI can help in predicting patient outcomes based on biopsy results, allowing for more personalized treatment plans.
Liquid biopsy is another innovative approach that involves analyzing circulating tumor DNA (ctDNA) or other biomarkers in the blood. This non-invasive method could provide valuable information about the presence of prostate cancer and its characteristics, reducing the need for invasive procedures like biopsies.
Furthermore, advancements in ultrasound technology, such as contrast-enhanced ultrasound and elastography, may improve the visualization of prostate tissue and enhance the accuracy of biopsy targeting. These techniques can provide real-time feedback during the biopsy procedure, allowing for better decision-making and potentially reducing complications.
In summary, the future of prostate cancer diagnosis may be significantly enhanced by these emerging technologies, leading to safer, more accurate, and less invasive diagnostic options for patients.
0
