FDA Approves Osimertinib, a Third-Generation EGFR Tyrosine Kinase Inhibitor, for Unresectable Non-Small Cell Lung Cancer
The US Food and Drug Administration (FDA) has approved the use of osimertinib (Tagrisso, AstraZeneca Pharmaceuticals), a third-generation epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor (TKI), for the treatment of locally advanced, unresectable non-small cell lung cancer (NSCLC) in certain adult patients.
Specifically, the approval is for patients whose disease has not progressed during or after concurrent or sequential platinum-based chemoradiation therapy and whose tumors have EGFR exon 19 deletions or exon 21 L858R mutations. These EGFR mutations can be detected by an FDA-approved test.
The FDA had previously approved osimertinib in combination with platinum-based chemotherapy as a first-line treatment for patients with locally advanced or metastatic NSCLC with the same EGFR mutations. The EGFR-TKI also carries other indications, including as first-line monotherapy for locally advanced or metastatic EGFR-mutated NSCLC.
The latest approval was based on findings from the randomized, placebo-controlled LAURA trial, which demonstrated improved median progression-free survival with osimertinib compared to placebo (39.1 vs 5.6 months; hazard ratio, 0.16). Overall survival results were still immature, but no trend towards a detriment was observed.
The most common adverse reactions reported in the study were lymphopenia, leukopenia, interstitial lung disease/pneumonitis, thrombocytopenia, neutropenia, rash, diarrhea, nail toxicity, musculoskeletal pain, cough, and COVID-19 infection.
Tilpas resumé
Genskriv med AI
Generer citater
Oversæt kilde
Til et andet sprog
Generer mindmap
fra kildeindhold
Besøg kilde
www.medscape.com
FDA Approves Osimertinib for Unresectable NSCLC
Vigtigste indsigter udtrukket fra
by Sharon Worce... kl. www.medscape.com 09-27-2024
https://www.medscape.com/viewarticle/fda-okays-osimertinib-after-crt-locally-advanced-2024a1000hjd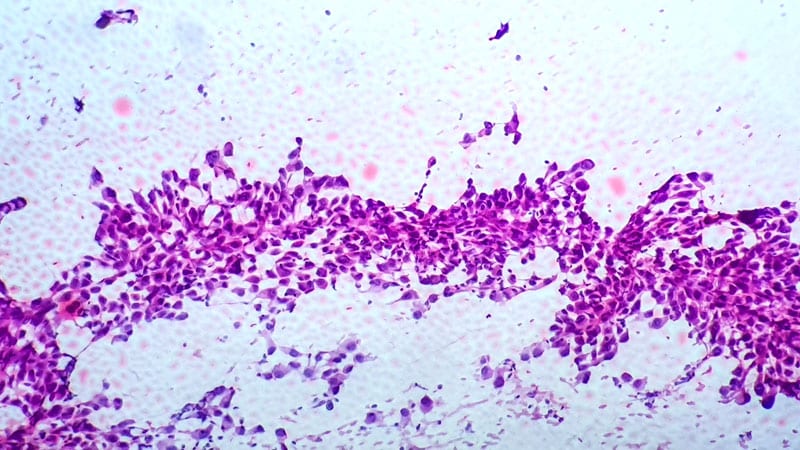
Dybere Forespørgsler
