Thrombectomy Benefits in Large-Strokes Revealed by Simple Imaging
Kernkonzepte
Endovascular thrombectomy significantly benefits acute ischemic stroke patients with large vessel occlusion and established large infarcts, as demonstrated by the TENSION trial.
Zusammenfassung
The TENSION trial showcased the substantial advantages of endovascular thrombectomy in acute ischemic stroke patients with large vessel occlusion and significant infarcts identified through basic imaging techniques. Here is a breakdown of the key points:
Trial Results:
- Thrombectomy led to an 18% increase in patients walking independently at 90 days.
- A mortality reduction of 11% at 90 days compared to medical therapy alone.
- Consistent benefits across all outcome categories and subgroups.
- No safety concerns or increase in intracranial hemorrhage with thrombectomy.
Study Details:
- Trial enrolled 665 patients with large vessel occlusion and extended infarcts.
- Patients randomly assigned to thrombectomy plus medical management or medical management alone.
- Early trial termination due to efficacy after enrolling 253 patients.
Outcome Analysis:
- Thrombectomy associated with better outcomes on the modified Rankin Scale.
- Significant improvement in functional independence and reduced mortality.
- No increase in severe hemorrhage with thrombectomy.
Expert Insights:
- Dr. Thomalla emphasized the life-saving potential of thrombectomy in this patient population.
- Dr. Nguyen highlighted the study's importance in treating patients with large ischemic core based on CT imaging alone.
Editorial Perspective:
- Dippel and Roozenbeek discussed the use of CT perfusion in patient selection for thrombectomy.
- Urged for meta-analyses to define patient populations benefiting from this treatment.
Zusammenfassung anpassen
Mit KI umschreiben
Zitate generieren
Quelle übersetzen
In eine andere Sprache
Mindmap erstellen
aus dem Quellinhalt
Quelle besuchen
www.medscape.com
Thrombectomy Benefits Large-Strokes After Simple Imaging
Statistiken
Thrombectomy resulted in an 18% absolute increase in patients walking independently at 90 days.
Mortality reduction of 11% at 90 days with thrombectomy.
Symptomatic intracranial hemorrhage occurred in 6% of patients with thrombectomy.
Zitate
"This pragmatic approach based on visual assessment of non-contrast CT yielded similar benefit to trials with more complicated and time-consuming imaging approaches." - Götz Thomalla
"In this population, thrombectomy really is saving lives. In this study, it saved the life of 1 patient in every 9 that were treated." - Götz Thomalla
Wichtige Erkenntnisse aus
by Sue Hughes um www.medscape.com 10-13-2023
https://www.medscape.com/viewarticle/997360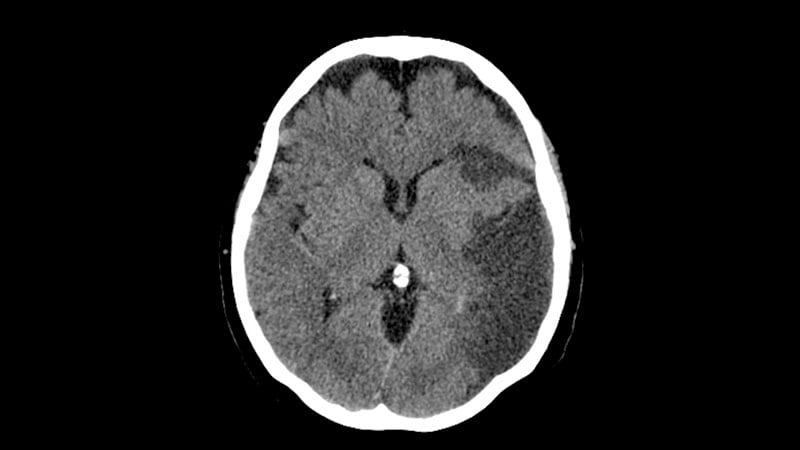
Tiefere Fragen
How can the findings of the TENSION trial impact the current guidelines for treating acute ischemic stroke patients?
The findings of the TENSION trial can have a significant impact on the current guidelines for treating acute ischemic stroke patients by potentially expanding the criteria for considering thrombectomy as a treatment option. The trial demonstrated that endovascular thrombectomy in patients with large vessel occlusion and a large infarct, identified through basic imaging techniques, led to improved functional outcomes and reduced mortality compared to medical therapy alone. These results suggest that patients with severe strokes and large infarcts, who would typically have a poor prognosis, could benefit from thrombectomy. Therefore, the findings may prompt a reevaluation of the current guidelines to include a broader range of patients who could benefit from this intervention.
What challenges might arise in implementing thrombectomy for patients with large infarcts based on basic imaging criteria?
Implementing thrombectomy for patients with large infarcts based on basic imaging criteria may pose several challenges. One challenge could be the need for healthcare providers to accurately identify patients who meet the criteria for thrombectomy based on non-contrast CT or CT angiography alone. This may require additional training and expertise to ensure proper patient selection. Another challenge could be the availability of resources and infrastructure to perform thrombectomy procedures in a timely manner for these patients. Since time is critical in stroke treatment, delays in accessing thrombectomy services could impact patient outcomes. Additionally, there may be concerns about the generalizability of the findings to different patient populations and healthcare settings, which could affect the widespread adoption of thrombectomy based on basic imaging criteria.
How can individual patient-data meta-analyses help optimize patient selection for endovascular thrombectomy in ischemic stroke treatment?
Individual patient-data meta-analyses can play a crucial role in optimizing patient selection for endovascular thrombectomy in ischemic stroke treatment by providing a comprehensive analysis of data from multiple trials. By combining data from various studies, researchers can identify patterns and trends in patient outcomes based on different criteria, such as imaging techniques, time windows, and patient characteristics. This approach allows for a more nuanced understanding of which patients are most likely to benefit from thrombectomy, leading to more precise guidelines for patient selection. Additionally, meta-analyses can help validate the findings of individual trials, especially those that are stopped early for efficacy, by providing a larger sample size and more robust statistical analysis. Overall, individual patient-data meta-analyses can contribute to evidence-based decision-making in optimizing patient selection for endovascular thrombectomy in ischemic stroke treatment.
0
