betekintés - Type 1 Diabetes Complications - # Diabetic Retinopathy Risk and Continuous Glucose Monitoring
Continuous Glucose Monitoring Associated with Lower Risk of Diabetic Retinopathy in Type 1 Diabetes
Alapfogalmak
The use of continuous glucose monitoring (CGM) is associated with a reduced risk of diabetic retinopathy and proliferative diabetic retinopathy in adults with type 1 diabetes.
Kivonat
This retrospective cohort study examined the association between the use of diabetes technologies, including continuous glucose monitoring (CGM) and insulin pumps, and the risk of diabetic retinopathy in adults with type 1 diabetes.
The key findings are:
- 44.4% of patients were diagnosed with diabetic retinopathy, with 11.1% and 49.2% having nonproliferative diabetic retinopathy with and without macular edema, respectively, and 11.9% and 27.9% having proliferative diabetic retinopathy with and without macular edema, respectively.
- Patients who used CGM had lower odds of diabetic retinopathy (OR 0.52, p=0.008) and lower odds of proliferative diabetic retinopathy (OR 0.42, p=0.004) compared to those who did not use CGM.
- The use of insulin pumps alone did not show an association with diabetic retinopathy, but the combined use of CGM and insulin pumps was associated with lower odds of proliferative diabetic retinopathy (OR 0.60, p=0.03) compared to no CGM or pump use.
- Among patients with more than one ophthalmology encounter who did not have proliferative diabetic retinopathy at baseline, only 21.8% experienced progression of diabetic retinopathy.
- Microvascular complications (OR 5.48, p<0.001) and higher mean A1c levels (OR 1.24, p=0.03) were associated with the risk of diabetic retinopathy progression.
The authors conclude that the use of CGM can support the prevention of diabetic retinopathy, particularly in high-risk groups.
Összefoglaló testreszabása
Átírás mesterséges intelligenciával
Hivatkozások generálása
Forrás fordítása
Egy másik nyelvre
Gondolattérkép létrehozása
a forrásanyagból
Forrás megtekintése
www.medscape.com
CGM Associated With Lower Retinopathy Risk in T1D
Statisztikák
44.4% of patients were diagnosed with diabetic retinopathy.
11.1% of patients had nonproliferative diabetic retinopathy with macular edema.
49.2% of patients had nonproliferative diabetic retinopathy without macular edema.
11.9% of patients had proliferative diabetic retinopathy with macular edema.
27.9% of patients had proliferative diabetic retinopathy without macular edema.
Patients who used CGM had lower odds of diabetic retinopathy (OR 0.52, p=0.008).
Patients who used CGM had lower odds of proliferative diabetic retinopathy (OR 0.42, p=0.004).
The combined use of CGM and insulin pumps was associated with lower odds of proliferative diabetic retinopathy (OR 0.60, p=0.03) compared to no CGM or pump use.
21.8% of patients with more than one ophthalmology encounter and no proliferative diabetic retinopathy at baseline experienced progression of diabetic retinopathy.
Microvascular complications (OR 5.48, p<0.001) and higher mean A1c levels (OR 1.24, p=0.03) were associated with the risk of diabetic retinopathy progression.
Idézetek
"CGM has a unique advantage that can support the prevention of diabetic retinopathy. This can be particularly beneficial in groups that are at the highest risk for retinal complications."
Főbb Kivonatok
by Manasi : www.medscape.com 04-05-2024
https://www.medscape.com/viewarticle/cgm-associated-lower-retinopathy-risk-t1d-2024a10006hw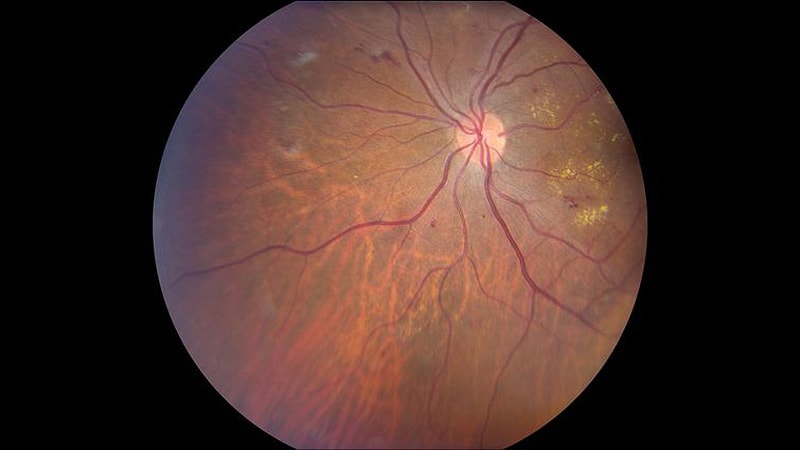
Mélyebb kérdések
How do the findings of this study compare to the impact of CGM on other microvascular complications in type 1 diabetes, such as nephropathy and neuropathy?
The findings of this study suggest that the use of continuous glucose monitoring (CGM) is associated with a reduced risk of diabetic retinopathy in adults with type 1 diabetes (T1D). When comparing these results to the impact of CGM on other microvascular complications like nephropathy and neuropathy, it is important to note that CGM has shown benefits beyond retinopathy. Previous research has indicated that CGM can also help in managing and reducing the risk of nephropathy and neuropathy in individuals with T1D. By providing real-time glucose data and trends, CGM can assist in maintaining tighter glycemic control, which is crucial in preventing various microvascular complications associated with diabetes.
What are the potential mechanisms by which CGM use may reduce the risk of diabetic retinopathy, and how can these insights be leveraged to improve diabetes management and prevent vision loss?
The potential mechanisms through which CGM use may reduce the risk of diabetic retinopathy involve the continuous monitoring of glucose levels, leading to better glycemic control. Fluctuations in blood sugar levels play a significant role in the development and progression of diabetic retinopathy. By providing individuals with real-time glucose data, CGM enables them to make immediate adjustments to their insulin dosages, diet, and lifestyle choices, thereby maintaining stable blood sugar levels. This consistent control helps in preventing the vascular damage that contributes to retinopathy. To leverage these insights for improved diabetes management and prevention of vision loss, healthcare providers can encourage the widespread adoption of CGM among individuals with T1D. Additionally, integrating CGM data with personalized treatment plans and patient education on interpreting and acting upon glucose trends can further enhance the benefits of CGM in reducing the risk of diabetic retinopathy.
Given the limitations of the study, such as potential selection bias and lack of generalizability, what additional research is needed to further validate the relationship between CGM use and diabetic retinopathy risk in diverse populations with type 1 diabetes?
To further validate the relationship between CGM use and diabetic retinopathy risk in diverse populations with type 1 diabetes, additional research is essential. Future studies should aim to address the limitations identified in this study by incorporating more diverse participant demographics, including individuals from different racial and socioeconomic backgrounds. Longitudinal studies with larger sample sizes can provide more robust evidence of the impact of CGM on diabetic retinopathy risk. Furthermore, research focusing on the specific mechanisms by which CGM influences retinopathy development, such as the role of glucose variability and time in range, can offer deeper insights into the benefits of CGM in preventing vision-related complications. Collaborative efforts between ophthalmologists, endocrinologists, and technology developers can help in designing comprehensive studies that explore the full potential of CGM in managing diabetic retinopathy across diverse populations with T1D.
0
