Muvalaplin Shows Promise in Lowering Lp(a) Cholesterol: Results from the Phase 2 KRAKEN Trial
This article reports the findings of the phase 2 KRAKEN trial, which investigated the efficacy and safety of muvalaplin, a new oral medication, in lowering lipoprotein(a) (Lp(a)) cholesterol levels.
High Lp(a): A Significant Cardiovascular Risk Factor
Lp(a) is a type of cholesterol whose levels are primarily determined by genetics and remain relatively stable throughout life. Elevated Lp(a) levels, 125 nmol/L or higher, are associated with an increased risk of heart attack, stroke, and other cardiovascular diseases. This particularly affects about 20% of the global population, with a higher prevalence among individuals of Black African and South Asian descent.
Muvalaplin: A Novel Therapeutic Approach
Currently, no approved therapies effectively lower Lp(a). While several injectable therapies are under clinical trials, muvalaplin stands out as the sole oral medication in development. The drug works by disrupting the bond within the Lp(a) particle, leading to its reduction.
KRAKEN Trial Design and Findings
The KRAKEN trial involved 233 adults with very high Lp(a) levels (> 175 nmol/L) who were randomly assigned to receive either one of three daily doses of muvalaplin (10, 60, or 240 mg) or a placebo for 12 weeks.
The study utilized both a standard blood test and a novel test specifically designed to measure intact Lp(a) particles. Results showed that muvalaplin significantly reduced Lp(a) levels compared to the placebo, with reductions of up to 70% with the standard test and up to 85.5% with the new test. Notably, approximately 82% of participants achieved an Lp(a) level below 125 nmol/L with the traditional test, and this figure rose to 97% with the new test. The 60 and 240 mg doses demonstrated similar efficacy, both surpassing the 10 mg dose. Importantly, muvalaplin was found to be safe and well-tolerated.
Expert Opinions and Future Directions
Experts view muvalaplin as a promising approach to addressing a previously untreatable condition. However, they emphasize the need for larger, longer-term studies with diverse patient populations to confirm these findings and determine whether Lp(a) reduction translates into improved cardiovascular outcomes.
Conclusion
The KRAKEN trial provides compelling evidence for the efficacy and safety of muvalaplin in lowering Lp(a) cholesterol. While further research is necessary, muvalaplin holds significant potential as a new therapeutic option for managing cardiovascular risk associated with elevated Lp(a) levels.
Kustomisasi Ringkasan
Tulis Ulang dengan AI
Buat Sitasi
Terjemahkan Sumber
Ke Bahasa Lain
Buat Peta Pikiran
dari konten sumber
Kunjungi Sumber
www.medscape.com
New Pill Successfully Lowers Lp(a) Levels
Wawasan Utama Disaring Dari
by Brian Owens pada www.medscape.com 11-19-2024
https://www.medscape.com/viewarticle/new-pill-successfully-lowers-lp-levels-2024a1000l13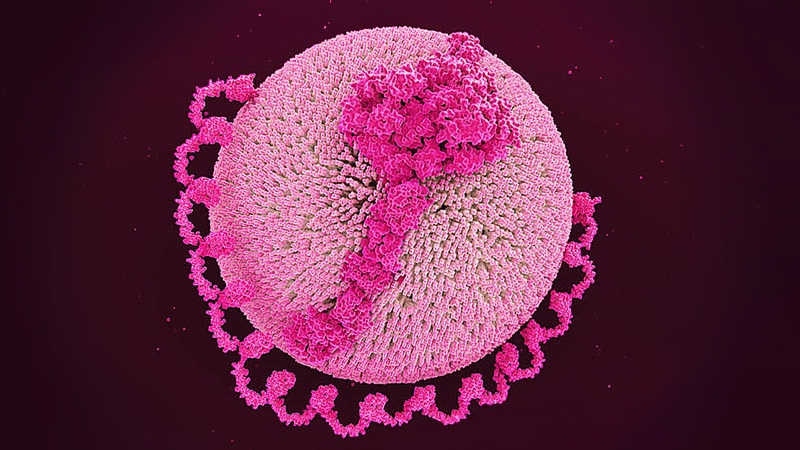
Pertanyaan yang Lebih Dalam
