insight - Medical Procedures - # Endoscopic Mucosal Resection Techniques for Large Colorectal Polyps
Comparative Safety and Efficacy of Cold Snare vs. Hot Snare Endoscopic Mucosal Resection for Large Colorectal Polyps
Core Concepts
Cold snare endoscopic mucosal resection (EMR) has a superior safety profile compared to hot snare EMR for large colorectal polyps, but may result in higher rates of residual adenoma and recurrence.
Abstract
This article reports the findings of the CHRONICLE trial, a randomized controlled study that compared the safety and efficacy of cold snare EMR versus hot snare EMR for the treatment of large (≥20 mm) colorectal polyps.
Key highlights:
- Major adverse events (perforation, post-endoscopic bleeding) were significantly lower in the cold snare group (1.0%) compared to the hot snare group (7.9%).
- Rates of perforation (0% vs. 3.9%) and post-procedural bleeding (1.0% vs. 4.4%) were also lower in the cold snare group.
- However, residual adenoma was found more frequently in the cold snare group (23.7%) compared to the hot snare group (13.8%).
- Polyp size was an independent predictor of major adverse events, residual adenoma, and high-grade dysplasia/cancer.
- For laterally spreading tumors (LSTs), the authors recommend hot snare EMR as the preferred treatment, while cold snare EMR may be an option for select cases of LST granular type homogenous and LST nongranular type without suspicion of malignancy.
- The authors conclude that while cold snare EMR has a superior safety profile, further research is needed to improve complete resection and minimize residual polyp rates.
Customize Summary
Rewrite with AI
Generate Citations
Translate Source
To Another Language
Generate MindMap
from source content
Visit Source
www.medscape.com
Cold Snare Resection Safe for Large Colorectal Polyps
Stats
Major adverse events occurred in 1.0% of the cold snare group and 7.9% of the hot snare group (p=0.001).
Perforation rates were 0% in the cold snare group and 3.9% in the hot snare group (p=0.007).
Post-procedural bleeding rates were 1.0% in the cold snare group and 4.4% in the hot snare group (p=0.040).
Residual adenoma was found in 23.7% of the cold snare group and 13.8% of the hot snare group (p=0.020).
Quotes
"Our study suggests that sessile serrated lesions larger than 2 cm should be resected with the cold snare. Selected cases of lateral spreading tumors may also be good candidates for cold snare resection when safety concerns are paramount."
"The higher recurrence rate after cold snare resection of LST nodular mixed types is unacceptable, and therefore, hot snare EMR with margin coagulation should be the treatment of choice."
Key Insights Distilled From
by Diana Swift at www.medscape.com 08-22-2024
https://www.medscape.com/viewarticle/cold-snare-resection-safe-large-nonpedunculated-colorectal-2024a1000fdo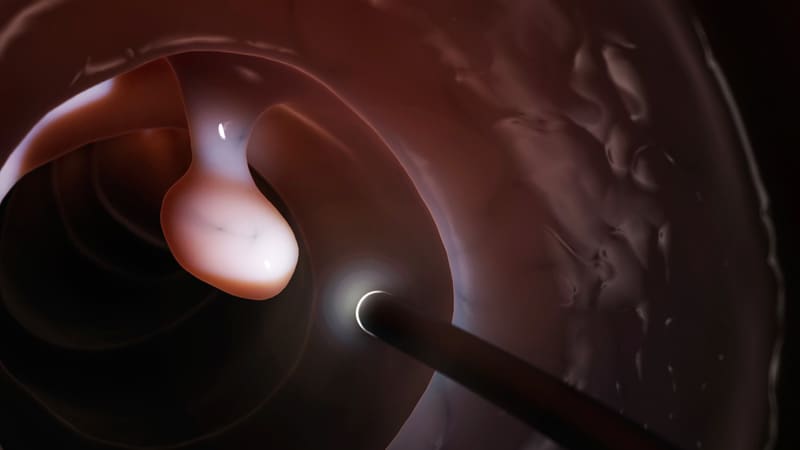
Deeper Inquiries
What technical innovations or additional measures could be explored to improve the complete resection rates and reduce residual polyp rates with cold snare EMR?
To enhance complete resection rates and decrease residual polyp rates with cold snare EMR, several technical innovations and additional measures could be explored. One approach could involve the development of advanced imaging technologies, such as high-definition endoscopy or virtual chromoendoscopy, to improve the visualization and delineation of polyp margins during the resection process. This enhanced visualization could aid in achieving more precise and complete resections, thereby reducing the likelihood of residual adenoma.
Furthermore, the integration of novel tools or accessories, such as submucosal injection agents or tissue retraction devices, may facilitate better maneuverability and control during cold snare EMR procedures. These tools could help in lifting the polyp, creating a clear operating field, and ensuring a more thorough resection without leaving residual tissue behind.
Additionally, the implementation of advanced hemostatic techniques, such as the use of hemostatic clips or thermal coagulation devices, could help manage any bleeding complications more effectively during the procedure. By improving hemostasis, these measures could contribute to a safer and more successful cold snare EMR with reduced rates of post-procedural bleeding.
How can patient selection criteria be further refined to identify the optimal candidates for cold snare EMR versus hot snare EMR for large colorectal polyps?
Refining patient selection criteria is crucial to identifying the optimal candidates for cold snare EMR versus hot snare EMR in the treatment of large colorectal polyps. One key aspect of patient selection involves considering the histological characteristics of the polyps, such as their size, morphology, and location within the colon. For instance, sessile serrated lesions larger than 2 cm and certain lateral spreading tumors may be more suitable for cold snare EMR when safety concerns are paramount.
Moreover, patient-specific factors, including comorbidities, bleeding risk, and preferences, should be taken into account when determining the most appropriate resection technique. Patients with a higher risk of bleeding complications or those who prefer a minimally invasive approach may benefit from cold snare EMR, whereas individuals with larger polyps or complex lesions may be better suited for hot snare EMR with margin coagulation.
By integrating both histological and patient-related criteria, clinicians can tailor the selection of resection techniques to each individual case, optimizing outcomes and minimizing risks associated with the procedure.
What are the long-term clinical outcomes and cost-effectiveness implications of adopting cold snare EMR as the primary treatment approach for large colorectal polyps in routine clinical practice?
The adoption of cold snare EMR as the primary treatment approach for large colorectal polyps in routine clinical practice has significant long-term clinical outcomes and cost-effectiveness implications. From a clinical perspective, utilizing cold snare EMR may lead to improved patient safety, as evidenced by lower rates of major adverse events, such as perforation and post-endoscopic bleeding, compared to hot snare EMR. This enhanced safety profile could result in reduced hospitalizations, complications, and healthcare costs associated with managing adverse events post-procedure.
However, the higher rates of residual adenoma and recurrence observed with cold snare EMR may necessitate closer surveillance and potentially additional interventions, impacting long-term clinical outcomes and follow-up care requirements. Clinicians would need to consider the implications of these findings on patient management strategies and the overall effectiveness of cold snare EMR in preventing disease recurrence.
In terms of cost-effectiveness, the upfront costs associated with implementing cold snare EMR, including equipment, training, and procedural time, should be weighed against the potential savings from reduced adverse events and post-procedural complications. Additionally, the need for surveillance colonoscopies and potential repeat procedures due to residual adenoma may influence the overall cost-effectiveness of cold snare EMR compared to alternative resection techniques.
Further research and real-world data are essential to evaluate the long-term clinical outcomes, patient satisfaction, and economic impact of adopting cold snare EMR as the primary treatment modality for large colorectal polyps, guiding clinical decision-making and healthcare resource allocation.
0
