Neuropeptide CGRP Signaling via RAMP3 Regulates T Helper Cell Differentiation and Antiviral Response
This research paper investigates the role of neuropeptide signaling in T cell differentiation, specifically focusing on the interplay between the neuropeptide CGRP and its receptor RAMP3.
Research Objective:
The study aimed to elucidate the mechanisms underlying the balance between TH1 and other T helper cell subsets, particularly during antiviral immune responses.
Methodology:
The researchers employed a multifaceted approach involving in vitro T cell polarization assays, CRISPR-Cas9 mediated gene editing for in vitro and in vivo screens, and a mouse model of acute viral infection.
Key Findings:
- RAMP3, a component of the CGRP receptor, was identified as a crucial regulator of TH1 cell fate determination.
- CGRP signaling through RAMP3 promoted TH1 cell differentiation while suppressing TH2 cell differentiation.
- Mechanistically, CGRP-RAMP3 signaling activated the transcription factors CREB and ATF3, with ATF3 directly inducing the expression of Stat1, a master regulator of TH1 cell differentiation.
- In vivo, during acute viral infection, neuronal CGRP production enhanced the differentiation of antiviral IFNγ-producing TH1 and CD8+ T cells, leading to efficient viral clearance.
Main Conclusions:
The study unveils a novel neuroimmune circuit where neuronal CGRP, released during viral infection, interacts with RAMP3 on T cells to promote TH1 cell differentiation and enhance antiviral immunity.
Significance:
This research significantly advances our understanding of the complex interplay between the nervous and immune systems, highlighting the role of neuropeptides in shaping adaptive immune responses.
Limitations and Future Research:
Further research is needed to explore the role of this pathway in chronic viral infections and other disease settings. Investigating the potential therapeutic implications of modulating CGRP-RAMP3 signaling in immune-related disorders is also warranted.
요약 맞춤 설정
AI로 다시 쓰기
인용 생성
소스 번역
다른 언어로
마인드맵 생성
소스 콘텐츠 기반
소스 방문
www.nature.com
Neuropeptide signalling orchestrates T cell differentiation - Nature
핵심 통찰 요약
by Yu Hou,Linyu... 게시일 www.nature.com 10-16-2024
https://www.nature.com/articles/s41586-024-08049-w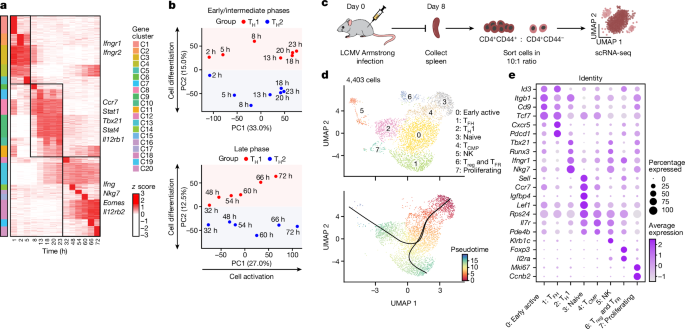
더 깊은 질문
