Comprehensive Single-Cell Analysis Reveals Age-Related Changes in Human Skeletal Muscle Composition and Molecular Profiles
Conceitos essenciais
Comprehensive single-cell and single-nucleus analysis of human skeletal muscle across different age groups reveals significant changes in cell populations and molecular profiles associated with sarcopenia and frailty in older individuals.
Resumo
The study presents a comprehensive single-cell/single-nucleus transcriptomic and chromatin accessibility map of human limb skeletal muscles from individuals aged 15 to 99 years with varying fitness and frailty levels. The key insights from the analysis are:
- Significant changes in cell population composition occur during aging, including the emergence of new cell types in older individuals.
- Cell-specific and multicellular network features at the transcriptomic and epigenetic levels are associated with these age-related changes.
- Cross-comparison with genetic data identifies key elements of chromatin architecture that mark susceptibility to sarcopenia, a common age-related condition characterized by muscle atrophy and functional decline.
- The study provides a valuable resource for understanding the molecular mechanisms underlying skeletal muscle aging and identifying potential targets for interventions to address sarcopenia and frailty in older adults.
Personalizar Resumo
Reescrever com IA
Gerar Citações
Traduzir Fonte
Para outro idioma
Gerar Mapa Mental
do conteúdo fonte
Visitar Fonte
www.nature.com
Multimodal cell atlas of the ageing human skeletal muscle - Nature
Estatísticas
The study analyzed over 387,000 cells/nuclei from human limb skeletal muscles across individuals aged 15 to 99 years.
Citações
"Muscle atrophy and functional decline (sarcopenia) are common manifestations of frailty and are critical contributors to morbidity and mortality in older people."
"Deciphering the molecular mechanisms underlying sarcopenia has major implications for understanding human ageing."
Principais Insights Extraídos De
by Yiwe... às www.nature.com 04-22-2024
https://www.nature.com/articles/s41586-024-07348-6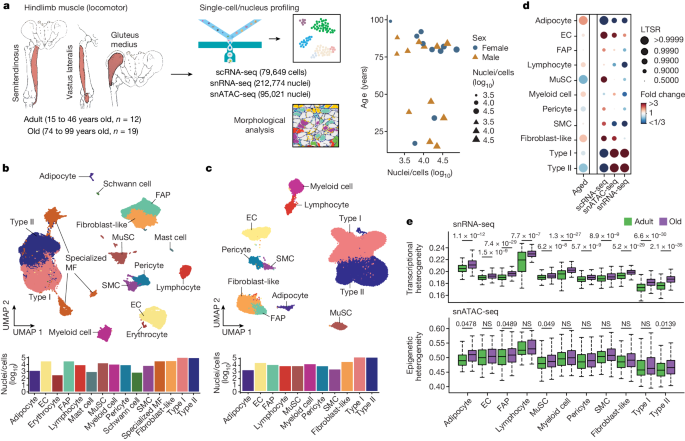
Perguntas Mais Profundas
How do the age-related changes in skeletal muscle cell populations and molecular profiles differ between individuals with varying levels of physical activity and fitness
The age-related changes in skeletal muscle cell populations and molecular profiles exhibit distinct patterns based on the levels of physical activity and fitness in individuals. Research has shown that individuals with higher levels of physical activity and fitness tend to have a more preserved muscle mass and function compared to sedentary individuals. In active and fit individuals, there is a tendency for a slower decline in muscle cell populations, such as satellite cells responsible for muscle repair and regeneration, compared to their sedentary counterparts. Additionally, physically active individuals often exhibit a more favorable molecular profile in their skeletal muscle, characterized by lower levels of inflammation, oxidative stress, and mitochondrial dysfunction, which are common features associated with sarcopenia and frailty in older adults. These individuals may also show enhanced expression of genes related to muscle growth, metabolism, and overall muscle health. On the other hand, sedentary individuals or those with lower fitness levels tend to experience a more rapid decline in muscle cell populations, increased inflammation, and altered gene expression patterns associated with muscle wasting and dysfunction. Therefore, the interplay between physical activity, fitness levels, and age-related changes in skeletal muscle highlights the importance of lifestyle factors in modulating the molecular and cellular processes underlying sarcopenia and frailty.
What are the potential limitations of the single-cell/single-nucleus approach in capturing the full complexity of the skeletal muscle niche, and how can these be addressed in future studies
While the single-cell/single-nucleus approach offers valuable insights into the heterogeneity of skeletal muscle cell populations, there are potential limitations that need to be considered. One limitation is the inability to capture the spatial organization and interactions between different cell types within the muscle tissue. This approach provides a snapshot of the cellular landscape but may not fully represent the dynamic and three-dimensional nature of the skeletal muscle niche. Additionally, the dissociation process required for single-cell/nucleus sequencing may lead to cell stress and altered gene expression profiles, potentially skewing the results. To address these limitations in future studies, integrating spatial transcriptomics techniques with single-cell sequencing can provide a more comprehensive understanding of the cellular composition and organization within the skeletal muscle tissue. Furthermore, advancements in imaging technologies, such as multiplexed imaging and spatial proteomics, can help visualize the spatial relationships between different cell types and their microenvironment, enhancing our understanding of the skeletal muscle niche complexity beyond transcriptomic and epigenetic analyses.
What are the potential therapeutic targets and lifestyle interventions that could be developed based on the insights from this study to mitigate the effects of sarcopenia and frailty in older adults
Based on the insights gained from the multimodal cell atlas of ageing human skeletal muscle, several potential therapeutic targets and lifestyle interventions can be identified to mitigate the effects of sarcopenia and frailty in older adults. Targeting key molecular pathways associated with muscle wasting and dysfunction, such as inflammation, oxidative stress, mitochondrial dysfunction, and impaired muscle regeneration, could lead to the development of pharmacological interventions aimed at preserving muscle mass and function in ageing individuals. For instance, drugs targeting specific inflammatory cytokines or pathways involved in mitochondrial biogenesis and function could help counteract the age-related decline in skeletal muscle health. Additionally, lifestyle interventions focusing on regular physical activity, resistance training, and adequate nutrition can play a crucial role in maintaining muscle mass and function in older adults. Personalized exercise programs tailored to individual fitness levels and health status can help prevent or delay the onset of sarcopenia and frailty. Moreover, promoting healthy lifestyle habits, such as balanced diet, adequate protein intake, and sufficient sleep, can complement pharmacological interventions and enhance the overall well-being of older adults. By targeting both molecular pathways and lifestyle factors, a multifaceted approach can be adopted to address the complex nature of sarcopenia and frailty in ageing populations.
0
