Endoscopic Measurement of Esophageal Mucosal Impedance Shows Promise for Accurate GERD Diagnosis
The content discusses a new endoscopic method for diagnosing gastroesophageal reflux disease (GERD) that measures esophageal mucosal impedance. The traditional gold standard for GERD diagnosis is impedance-pH monitoring, which can be costly, not widely available, and requires the patient to wear a catheter for 24 hours.
The study, conducted in Brazil, evaluated 60 patients with typical GERD symptoms. All patients underwent impedance-pH monitoring, which was used as a reference to assess esophageal mucosal impedance via catheter during endoscopy. Measurements were taken at 4 different locations above the esophagogastric junction.
The results showed that patients without GERD, as determined by impedance-pH monitoring, exhibited significantly higher mucosal impedance values when measured during endoscopy at 2 and 5 cm above the esophagogastric junction. The highest sensitivity (96.4%) and specificity (87.5%) for ruling out GERD came from measurements taken at 2 cm.
The researchers explained that lower mucosal impedance indicates greater tissue permeability, which likely signifies more damage from reflux. They found that impedance values higher than 2970 Ω at 2 cm from the esophagogastric junction were indicative of excluding GERD.
While this endoscopic method is promising, it is not yet ready for widespread clinical use and requires further adaptations and validation by other research groups. The method may offer advantages over traditional techniques, such as assessing chronic damage-related permeability rather than just the patient's condition on the day of the test.
Özeti Özelleştir
Yapay Zeka ile Yeniden Yaz
Alıntıları Oluştur
Kaynağı Çevir
Başka Bir Dile
Zihin Haritası Oluştur
kaynak içeriğinden
Kaynak
www.medscape.com
New Endoscopic Method for GERD Diagnosis Shows High Accuracy
Önemli Bilgiler Şuradan Elde Edildi
by Teresa Santo... : www.medscape.com 09-19-2024
https://www.medscape.com/viewarticle/new-endoscopic-method-gerd-diagnosis-shows-high-accuracy-2024a1000h29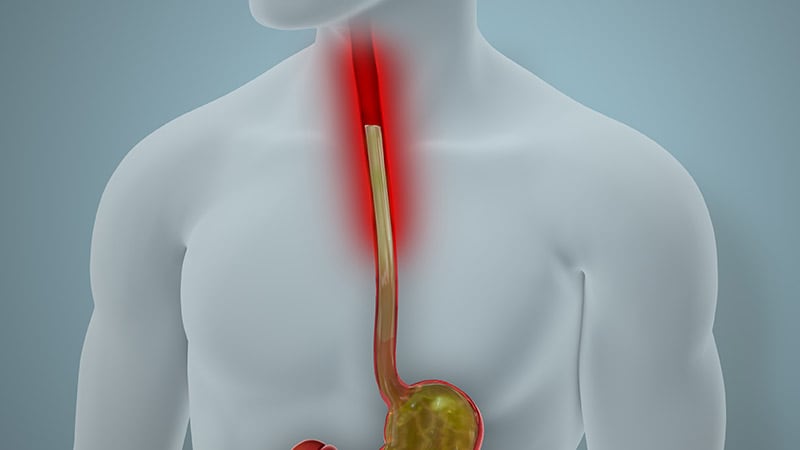
Daha Derin Sorular
