Gut Microbiome Impact on Heart Failure Therapy
核心概念
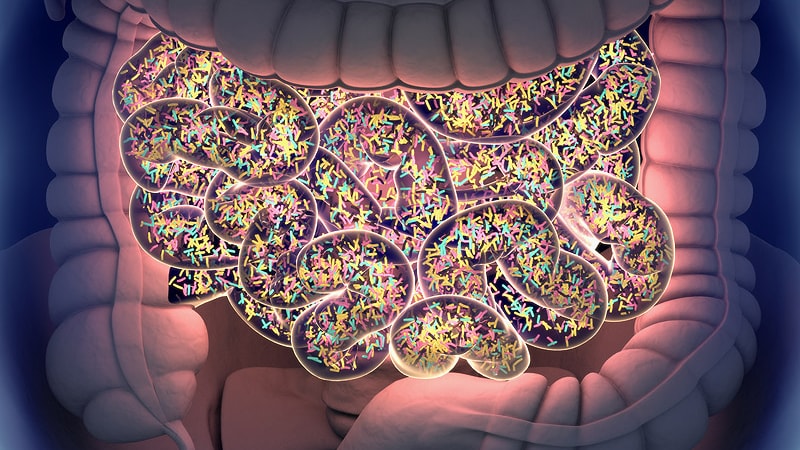
Understanding the gut microbiome's impact on heart failure can lead to personalized therapies.
摘要
The content discusses the significant role of the gut microbiome in influencing heart failure development and treatment. It emphasizes the potential for personalized approaches in managing the condition based on microbiome interactions, diet, and medications. Key insights include:
- Gut microbiome modulates heart failure pathophysiology.
- Diet and medications offer innovative modalities for heart failure management.
- Microbiome alterations in cardiovascular diseases.
- Impact of microbial products on heart recovery and blood pressure.
- Role of short-chain fatty acids in heart protection.
- Effects of trimethylamine N-oxide on cardiac remodeling.
- Benefits of high-fiber diets in heart failure.
- Personalization of diet and treatments based on microbiome composition.
- Potential of microbiome-targeting therapies in heart failure treatment.
- Importance of probiotics in altering host physiology.
- Need for more research on microbiome data collection and analysis.
客製化摘要
使用 AI 重寫
產生引用格式
翻譯原文
翻譯成其他語言
產生心智圖
從原文內容
前往原文
www.medscape.com
Gut Microbiome May Guide Personalized Heart Failure Therapy
統計資料
"The gut microbiome modulates heart failure pathophysiology, contributes to disease progression and therapeutic responses, and holds promise as a novel biomarker."
"In heart failure, the gut microbes that make these short-chain fatty acids are significantly depleted."
"Some of our preliminary data have shown people who have heart failure have severely depleted Bifidobacteria."
引述
"The gut microbiome modulates heart failure pathophysiology, contributes to disease progression and therapeutic responses, and holds promise as a novel biomarker."
"In heart failure, the gut microbes that make these short-chain fatty acids are significantly depleted."
"Some of our preliminary data have shown people who have heart failure have severely depleted Bifidobacteria."
深入探究
How can the microbiome data be effectively integrated into personalized heart failure therapies?
Microbiome data can be effectively integrated into personalized heart failure therapies by first understanding the unique composition of an individual's gut microbiome. This involves analyzing the specific bacteria present, their functionality, and how they interact with the host. By collecting stool samples and combining this data with information on metabolites, cytokines, diet, medication, and clinical outcomes, healthcare providers can tailor treatment plans to each patient. For example, identifying which bacteria are depleted or overrepresented in a patient with heart failure can guide the use of targeted probiotics or dietary interventions to restore a healthy microbiome balance. Additionally, monitoring changes in the microbiome over time can help predict treatment responses and optimize therapy for better outcomes.
What are the potential drawbacks or limitations of relying on probiotics for heart failure treatment?
While probiotics show promise in modulating the gut microbiota and improving cardiac function in some cases, there are several drawbacks and limitations to consider when relying on them for heart failure treatment. One limitation is the lack of regulation in the probiotics market, leading to variability in product quality and efficacy. Not all probiotics contain the specific strains of bacteria needed to address the dysbiosis associated with heart failure. Additionally, the effects of probiotics can vary widely among individuals due to differences in microbiome composition and response to specific bacterial strains. Furthermore, the evidence supporting the use of probiotics in heart failure is still limited, with mixed results from clinical trials. More research is needed to determine the optimal probiotic formulations, dosages, and duration of treatment for heart failure patients.
How might advancements in microbiome research impact other areas of healthcare beyond heart failure management?
Advancements in microbiome research have the potential to revolutionize healthcare across various medical specialties beyond heart failure management. By gaining a deeper understanding of how the gut microbiome influences overall health and disease, personalized therapies can be developed for conditions ranging from inflammatory bowel disease to mental health disorders. Microbiome-targeting therapies may become integral in treating conditions such as obesity, diabetes, autoimmune diseases, and even cancer. The ability to analyze and manipulate the microbiome opens up new avenues for preventive medicine, diagnostic tools, and therapeutic interventions. As research progresses, microbiome data could be routinely included in biobanks, providing valuable insights into individual health profiles and guiding personalized treatment strategies across diverse healthcare fields.
0
