Challenging the Status Quo in Gynecological Cancer Surgery: An Interview with Andreas Obermair
The interview with Andreas Obermair, a renowned gynecological cancer surgeon, highlights the need to critically examine the evidence behind clinical practice guidelines in the field of gynecological cancer surgery. Obermair argues that many guidelines are based on weak data and do not adequately consider the patient's perspective, resulting in poor quality-of-life outcomes.
Obermair has been involved in several practice-changing studies, such as the LACC trial, which demonstrated that minimally invasive radical hysterectomy was associated with lower rates of disease-free survival and overall survival compared to open abdominal radical hysterectomy in early-stage cervical cancer. He is currently planning to conduct the ENDO-3 trial, which aims to offer an alternative treatment pathway in endometrial cancer beyond the prevailing standard of surgical staging.
Obermair also discusses the ANVU trial, which he is involved in as an investigator. This trial is designed to explore whether intensive groin ultrasound monitoring can be a safe and cost-effective replacement for invasive groin lymph node dissection in vulvar cancer, potentially decreasing the associated morbidity.
Obermair emphasizes the importance of using high-quality data to inform guidelines and the need to consider the patient's perspective. He criticizes the "complacency" in the field, where clinicians often adhere to guidelines without questioning the underlying evidence or exploring alternative treatment options that may lead to better outcomes for patients.
The interview highlights the challenges in conducting surgical clinical trials, as funding is often difficult to secure compared to medical trials. Obermair argues that this barrier contributes to the lack of strong evidence supporting some guidelines, which can lead to suboptimal care.
Overall, the interview underscores the need for clinicians to be proactive in challenging the status quo, conducting rigorous research, and incorporating the patient's voice to improve the quality of care in gynecological cancer surgery.
Tùy Chỉnh Tóm Tắt
Viết Lại Với AI
Tạo Trích Dẫn
Dịch Nguồn
Sang ngôn ngữ khác
Tạo sơ đồ tư duy
từ nội dung nguồn
Xem Nguồn
www.medscape.com
Q&A With Andreas Obermair
Thông tin chi tiết chính được chắt lọc từ
by Whitney lúc www.medscape.com 09-20-2024
https://www.medscape.com/viewarticle/andreas-obermair-gynecological-cancer-surgery-guidelines-2024a1000h4b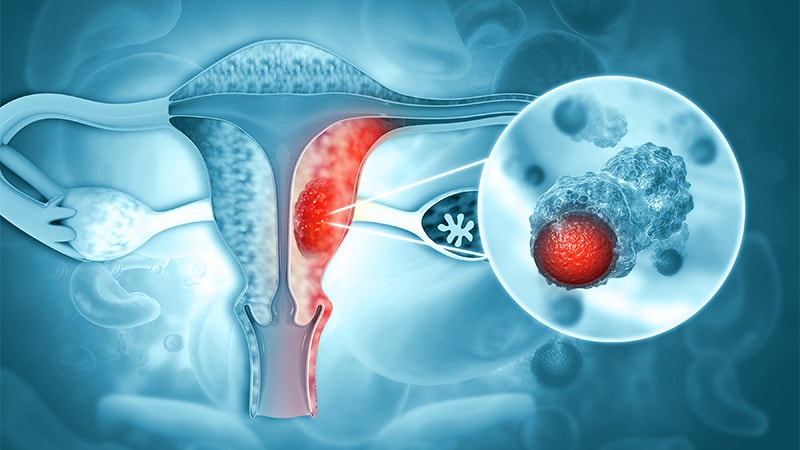
Yêu cầu sâu hơn
