indsigt - Rheumatology - # Predicting Interstitial Lung Disease Risk in Systemic Sclerosis Patients Using Anti-Ro/SSA Antibodies
Anti-Ro/SSA Antibodies Linked to Higher Risk of Interstitial Lung Disease in Systemic Sclerosis Patients
Kernekoncepter
Anti-Ro/SSA antibodies are an independent risk factor for interstitial lung disease in patients with systemic sclerosis, but do not predict disease progression or survival.
Resumé
This study analyzed data from a large European cohort of systemic sclerosis (SSc) patients to investigate the potential of anti-Ro/SSA antibodies as a biomarker for predicting interstitial lung disease (ILD) risk.
Key findings:
- 15% of SSc patients in the cohort tested positive for anti-Ro/SSA antibodies.
- Patients positive for anti-Ro/SSA antibodies had a higher prevalence of ILD (56.2% vs. 47.8%) and lower diffusing capacity of the lungs for carbon monoxide (DLCO%) at baseline.
- After adjusting for known risk factors, the researchers found that anti-Ro/SSA antibodies are an independent risk factor for ILD, with an odds ratio of 1.24.
- Anti-Ro/SSA antibodies were also associated with lower DLCO% in patients with established ILD.
- However, anti-Ro/SSA antibodies did not predict the progression of ILD, overall disease progression, or survival during the follow-up period.
The researchers suggest that anti-Ro/SSA antibodies could be incorporated into routine clinical practice to help identify SSc patients at high risk of developing ILD, particularly in settings where high-resolution computed tomography (HRCT) is not readily available.
Tilpas resumé
Genskriv med AI
Generer citater
Oversæt kilde
Til et andet sprog
Generer mindmap
fra kildeindhold
Besøg kilde
www.medscape.com
Anti-Ro/SSA Antibodies Have Potential to Predict ILD in SSc
Statistik
15% of all SSc patients presented as positive for anti-Ro/SSA antibodies.
ILD was present in 56.2% of patients positive for anti-Ro/SSA antibodies and in 47.8% of those who were negative (P = .001).
FVC% was 92.5% in patients positive for anti-Ro/SSA antibodies and 95.7% in those who were negative (P = .002).
DLCO% was 66.9% in patients positive for anti-Ro/SSA antibodies and 71% in those who were negative (P < .001).
After adjusting for known risk factors, anti-Ro/SSA antibodies were found to be an independent risk factor for ILD, with an odds ratio of 1.24 (95% CI, 1.07-1.44; P = .006).
Anti-Ro/SSA antibodies were a risk factor for lower DLCO values in patients with ILD, with a regression coefficient of −1.93.
Citater
"A total of 15% of all SSc patients presented as positive for anti-Ro/SSA antibodies, and these patients all presented with higher prevalence of SSA-nonspecific antibodies, too: Of note, those with anti-La/SSB and anti-U1/RNP and rheumatoid factor."
"Anti-Ro/SSA-positive patients with established ILD at baseline presented with lower DLCO values at 59% in patients positive for anti-Ro/SSA antibodies and 61% for those who were negative."
Vigtigste indsigter udtrukket fra
by Becky Mccall kl. www.medscape.com 06-14-2024
https://www.medscape.com/viewarticle/anti-ro-ssa-antibodies-have-potential-predict-ild-systemic-2024a1000b4m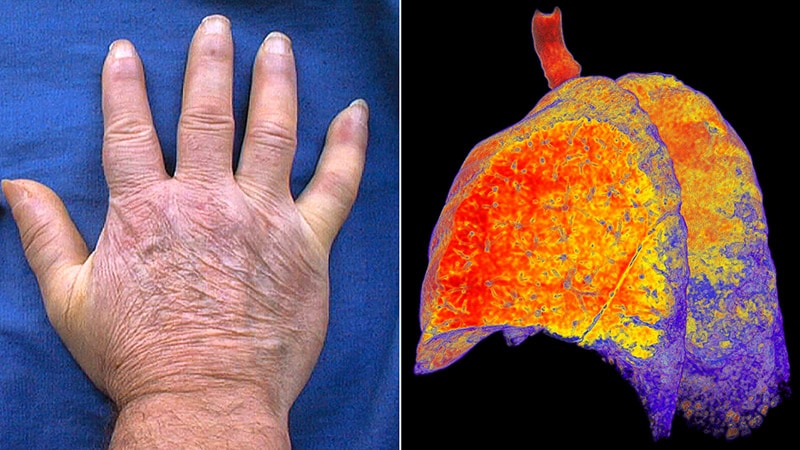
Dybere Forespørgsler
What are the potential mechanisms by which anti-Ro/SSA antibodies contribute to the development of interstitial lung disease in systemic sclerosis patients?
Anti-Ro/SSA antibodies are believed to play a role in the pathogenesis of interstitial lung disease (ILD) in systemic sclerosis (SSc) patients through several potential mechanisms. These antibodies are known to target intracellular antigens, specifically the Ro52 and Ro60 proteins, which are involved in RNA metabolism and protein synthesis. When these antibodies are present, they can lead to immune complex formation and subsequent activation of inflammatory pathways, contributing to tissue damage and fibrosis in the lungs. Additionally, anti-Ro/SSA antibodies have been associated with increased levels of proinflammatory cytokines and chemokines, which can further promote inflammation and fibrosis in the lung tissue. Overall, the presence of anti-Ro/SSA antibodies may trigger an autoimmune response that leads to the development and progression of ILD in SSc patients.
How can the findings of this study be used to improve the clinical management and monitoring of systemic sclerosis patients at risk of developing interstitial lung disease?
The findings of this study suggest that anti-Ro/SSA antibodies can serve as a valuable biomarker for predicting the risk of interstitial lung disease (ILD) in systemic sclerosis (SSc) patients. By incorporating the assessment of these antibodies into routine clinical practice, healthcare providers can better identify patients who are at a higher risk of developing ILD. This information can guide screening efforts, especially in settings where high-resolution computed tomography (HRCT) may not be readily available. Early detection of ILD in SSc patients can lead to timely interventions and closer monitoring of lung function, potentially improving outcomes and quality of life for these individuals. Additionally, the study highlights the importance of considering nonspecific autoantibodies, such as anti-Ro/SSA antibodies, in risk stratification and personalized management of SSc patients with lung involvement.
Given the limitations of the study, what additional research is needed to further validate the use of anti-Ro/SSA antibodies as a biomarker for predicting interstitial lung disease in systemic sclerosis?
While the study provides valuable insights into the potential role of anti-Ro/SSA antibodies as a biomarker for predicting interstitial lung disease (ILD) in systemic sclerosis (SSc), there are several limitations that warrant further research to validate these findings. Future studies should aim to address the lack of standardized criteria for assessing anti-Ro/SSA positivity across different centers, as this could impact the consistency and reliability of the results. Additionally, distinguishing between anti-Ro52 and anti-Ro60 subtypes may provide more specific information on the association between these antibodies and ILD in SSc patients. Standardized criteria for evaluating lung progression in SSc, as well as larger longitudinal studies with extended follow-up periods, could help confirm the predictive value of anti-Ro/SSA antibodies in identifying patients at risk of ILD development and progression. Further research is also needed to explore the underlying mechanisms by which these antibodies contribute to lung fibrosis and to investigate potential therapeutic targets based on these findings.
0
