Uncovering the Immune-Neuronal Axis Controlling Allergic Responses: A γδ T Cell–IL-3 Signaling Pathway Regulates Sensory Neuron Activation by Allergens
Alapfogalmak
A γδ T cell-derived cytokine, IL-3, acts on sensory neurons to lower their activation threshold to allergens, thereby promoting the initiation of allergic immune responses.
Kivonat
The article explores the bidirectional neuroimmune circuits that drive allergic responses, focusing on how immune cells regulate the sensitivity of sensory neurons to allergens in the naive state. The key findings are:
A specific subset of epidermal γδ T cells, termed GD3 cells, produces the cytokine IL-3 and promotes allergic itch and the initiation of the allergic immune response.
IL-3 acts on sensory neurons expressing the IL-3 receptor (Il3ra) in a JAK2-dependent manner, lowering their threshold for activation by allergens without directly eliciting itch.
The γδ T cell-IL-3 signaling axis further acts through the STAT5 pathway to promote neuropeptide production and the initiation of allergic immunity.
This immune-neuronal regulatory pathway may explain individual differences in allergic susceptibility and offers new therapeutic avenues for treating allergic diseases.
A γδ T cell–IL-3 axis controls allergic responses through sensory neurons - Nature
Statisztikák
"In naive individuals, sensory neurons directly detect and respond to allergens, leading to both the sensation of itch and the activation of local innate immune cells, which initiate the allergic immune response."
"We define a poorly characterized epidermal γδ T cell subset8, termed GD3 cells, that produces its hallmark cytokine IL-3 to promote allergic itch and the initiation of the allergic immune response."
"IL-3 acts on Il3ra-expressing sensory neurons in a JAK2-dependent manner to lower their threshold for allergen activation without independently eliciting itch."
"This γδ T cell–IL-3 signalling axis further acts by means of STAT5 to promote neuropeptide production and the initiation of allergic immunity."
Idézetek
"This pathway may explain individual differences in allergic susceptibility and opens new therapeutic avenues for treating allergic diseases."
Főbb Kivonatok
by Cameron H. F... : www.nature.com 09-04-2024
https://www.nature.com/articles/s41586-024-07869-0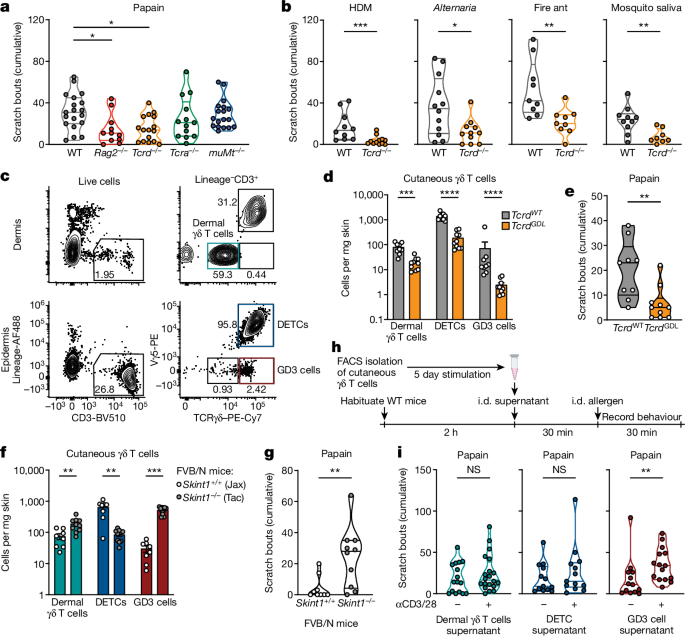
Mélyebb kérdések
How might the γδ T cell-IL-3 signaling axis be leveraged to develop novel therapies for allergic diseases?
The γδ T cell-IL-3 signaling axis presents a promising target for the development of novel therapies aimed at allergic diseases. By understanding the role of γδ T cells, particularly the GD3 subset, in producing IL-3, researchers can explore strategies to modulate this pathway. One potential therapeutic approach could involve the use of IL-3 antagonists or inhibitors that specifically block the interaction between IL-3 and its receptor on sensory neurons. This could effectively raise the threshold for allergen activation, thereby reducing the sensation of itch and the initiation of the allergic immune response. Additionally, therapies that enhance the regulatory functions of γδ T cells could be developed to promote a balanced immune response, potentially mitigating the severity of allergic reactions. Furthermore, the identification of small molecules or biologics that can selectively target the JAK2-STAT5 signaling cascade activated by IL-3 may provide another avenue for intervention, allowing for the fine-tuning of sensory neuron responsiveness to allergens without compromising overall immune function.
What other immune cell types or signaling pathways could potentially modulate the sensitivity of sensory neurons to allergens?
Beyond γδ T cells, several other immune cell types and signaling pathways may influence the sensitivity of sensory neurons to allergens. For instance, mast cells, which are known to play a critical role in allergic responses, release various mediators such as histamine and cytokines that can sensitize sensory neurons and exacerbate itch. Additionally, T helper (Th) cells, particularly Th2 cells, produce cytokines like IL-4 and IL-13 that can enhance the allergic response and potentially modulate neuronal sensitivity. The interplay between these immune cells and sensory neurons may involve complex signaling networks, including the involvement of neuropeptides such as substance P and calcitonin gene-related peptide (CGRP), which are released by sensory neurons and can further amplify the immune response. Other pathways, such as the neuroimmune interactions mediated by the vagus nerve, may also play a role in modulating sensory neuron sensitivity to allergens, highlighting the multifaceted nature of the immune-neuronal axis in allergic diseases.
What are the broader implications of this immune-neuronal regulatory mechanism for our understanding of the interplay between the nervous and immune systems in health and disease?
The discovery of the γδ T cell-IL-3 signaling axis as a regulator of sensory neuron responsiveness to allergens underscores the intricate interplay between the nervous and immune systems. This immune-neuronal regulatory mechanism suggests that sensory neurons are not merely passive responders to immune signals but are active participants in shaping immune responses. Such insights could revolutionize our understanding of various conditions beyond allergies, including chronic pain, autoimmune diseases, and neuroinflammatory disorders, where similar neuroimmune interactions may be at play. Furthermore, this mechanism highlights the potential for developing therapies that target these interactions, paving the way for innovative treatments that address the root causes of diseases rather than just their symptoms. Understanding how immune cells like γδ T cells communicate with sensory neurons could also lead to the identification of biomarkers for allergic susceptibility and the development of personalized medicine approaches tailored to individual immune-neuronal profiles. Overall, this research emphasizes the need for a holistic view of health that considers the dynamic relationships between the nervous and immune systems.
0
