Strategies to Increase Colorectal Cancer Screening Rates: Offering Choices, Targeted Outreach, and Systematic Approaches
Core Concepts
Implementing a systematic, multi-pronged approach that includes offering patients screening options, targeted outreach to newly eligible individuals, and coordinated care between primary care and gastroenterology can significantly increase colorectal cancer screening rates.
Abstract
The article discusses various strategies to improve colorectal cancer (CRC) screening rates, which have remained below public health goals in the United States. Key insights include:
-
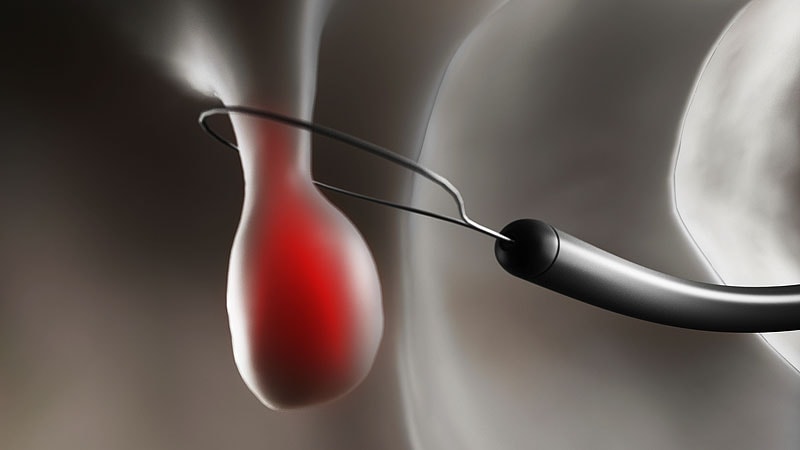
Offering patients a choice between colonoscopy and stool-based screening (e.g., fecal immunochemical test, FIT) can increase screening completion rates. Providing informational materials and making the process easy for patients are crucial.
-
Targeting newly eligible patients (ages 50-51) for screening outreach can be more effective than reaching out to those who are already behind on screening. Newly eligible patients are more likely to complete testing compared to the older, "more refractory" group.
-
Implementing a systematic, multi-faceted approach is essential. This includes embedding reminders in electronic health records, providing patient navigators, reducing structural barriers, and coordinating care between primary care and gastroenterology to ensure appropriate follow-up for patients with positive FIT results.
-
While colonoscopy has been the gold standard, stool-based tests like FIT can be more appealing to patients and lead to similar cancer detection and mortality reduction rates due to higher participation rates.
-
The responsibility of increasing screening rates should not fall solely on individual clinicians, but rather on changing the way the entire clinic operates through evidence-based interventions.
Translate Source
To Another Language
Generate MindMap
from source content
Visit Source
www.medscape.com
Colorectal Cancer Screening: How to Increase Rates
Stats
Only 72% of adults between ages 50 and 75 years were up-to-date on CRC screening by 2021.
In the study, 5.6% of the patients in the colonoscopy-only arm had obtained screening compared with 11.3% in the group offered FIT only and 12.8% of patients given a choice of modalities.
In the previous trial, patients who received a letter recommending they call their provider to schedule a colonoscopy were less likely to obtain screening than those who were initially mailed a FIT kit or who received the kit in the mail a month after not responding to the initial letter.
The study found newly eligible patients (ages 50-51) were more likely to complete testing (58%) than patients aged 52 years and above who were behind on testing (41%).
Quotes
"Making it really easy for patients to participate, whether it's through sending them reminders, or mailing people fit kits, or making the scheduling process for completing colonoscopy easier."
"We know that in the absence of any organized approach to screening, we allow people to fall through the cracks."
"Any test is better than no test."
Deeper Inquiries
How can healthcare systems effectively leverage digital data and electronic medical records to identify and proactively reach out to individuals who are due for colorectal cancer screening?
Healthcare systems can effectively leverage digital data and electronic medical records by implementing systematic approaches to identify individuals who are due for colorectal cancer screening. By utilizing data collected in electronic medical record systems, healthcare providers can track when patients last had screening tests like FIT or colonoscopy. This information can then be used to send targeted reminders and outreach to patients who are overdue for screening. Automated systems can be set up to generate reminders for patients, making it easier for healthcare providers to reach out to a large number of individuals efficiently. By leveraging digital data, healthcare systems can ensure that individuals are not falling through the cracks and are receiving timely reminders and information about the importance of colorectal cancer screening.
What are the potential barriers and drawbacks of relying solely on patient choice and preference for screening modalities, and how can they be addressed?
While offering patients a choice in screening modalities can increase participation rates, there are potential barriers and drawbacks to relying solely on patient choice. One drawback is that patients may not have enough information or understanding about the different screening options to make an informed decision. This lack of knowledge can lead to confusion and indecision, ultimately resulting in lower screening rates. Additionally, some patients may have personal preferences or biases that could influence their choice of screening modality, potentially leading to suboptimal screening outcomes.
To address these barriers and drawbacks, healthcare providers can implement educational initiatives to ensure that patients are well-informed about the various screening options available. Providing clear and accessible information about the pros and cons of each screening modality can help patients make informed decisions based on their individual preferences and risk factors. Healthcare providers can also offer guidance and support to patients in selecting a screening modality that aligns with their needs and preferences, ultimately leading to higher participation rates and better screening outcomes.
What innovative approaches or technologies could be explored to further improve colorectal cancer screening rates, especially among underserved or hard-to-reach populations?
To further improve colorectal cancer screening rates, especially among underserved or hard-to-reach populations, healthcare providers can explore innovative approaches and technologies. One approach is the use of telehealth and mobile health technologies to provide remote screening options for individuals who may have limited access to healthcare facilities. Telehealth platforms can offer virtual consultations, educational resources, and even at-home screening kits to increase accessibility and convenience for underserved populations.
Additionally, community outreach programs and partnerships with community organizations can help raise awareness about the importance of colorectal cancer screening and provide support to individuals in underserved areas. By collaborating with local clinics, community centers, and advocacy groups, healthcare providers can reach a wider audience and address barriers to screening such as transportation issues or lack of insurance coverage.
Furthermore, the development of AI-driven screening tools and predictive analytics can help identify individuals at higher risk for colorectal cancer and target interventions accordingly. By leveraging technology to personalize screening recommendations and outreach efforts, healthcare providers can improve screening rates and ultimately reduce the burden of colorectal cancer in underserved populations.