Benefits and Limitations of Stroke Thrombectomy in Low-Income Populations
Core Concepts
Thrombectomy in low-income populations can be beneficial without advanced imaging but may not benefit older patients due to frailty.
Abstract
The RESILIENT-Extend trial conducted in Brazil explored the benefits of thrombectomy in the late time window for stroke patients. Key highlights include:
Simplified selection criteria based on non-contrast CT
Potential alteration of current guidelines
Lack of benefit in older patients due to frailty
Bidirectional results on modified Rankin Scale
Increased chances of good outcomes with thrombectomy
Concerns about increased risk for severe disability or death
Importance of considering specific populations and factors like socioeconomic status and frailty
Potential ceiling effect for benefit of thrombectomy in frail patients
Absolute benefit of thrombectomy but also a signal of harm
Physiological differences in patients compared to other trials
Positive impact on extending access to thrombectomy in resource-limited settings
Expanded Window of Stroke Thrombectomy With Simpler Imaging
Stats
"The trial enrolled 245 patients with a large vessel occlusion stroke within 8-24 hours of last known well."
"The median baseline NIHSS score was 16, and the median ASPECTS score was 7-8."
"The number of patients achieving a good outcome (mRS, 0-2) was significantly increased with thrombectomy (25% vs 14%, adjusted odds ratio, 2.56; P = .012)."
Quotes
"The RESILIENT-Extend trial is the first major study of thrombectomy in the late time window (8-24 h) conducted outside first world countries and shows the procedure also has benefit in a lower socioeconomic status population without the need for costly imaging equipment." - Raul G. Nogueira, MD
"Both the RESILIENT trials have shown that thrombectomy does not appear to be suitable for older patients (over 68-70) years of age in the public health service in Brazil." - Raul G. Nogueira, MD
Key Insights Distilled From
by at www.medscape.com 02-09-2024
https://www.medscape.com/viewarticle/expanded-window-stroke-thrombectomy-simpler-imaging-2024a10002w4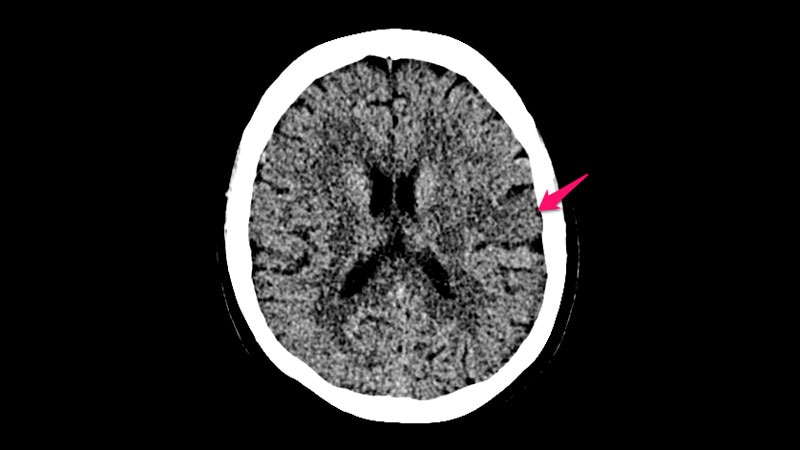
Deeper Inquiries
What are the implications of the bidirectional results on the modified Rankin Scale for future thrombectomy procedures?
The bidirectional results on the modified Rankin Scale (mRS) from the RESILIENT-Extend trial have significant implications for future thrombectomy procedures. While thrombectomy increased the chances of a good or excellent outcome (mRS 0-3), there was also a nonsignificant increased risk for a bad outcome (mRS 5-6). This bidirectional effect complicates the interpretation of the primary endpoint and suggests that the procedure may not universally benefit all patients. Future thrombectomy procedures need to carefully consider the potential for both positive and negative outcomes, especially in specific patient populations like those in low-income settings where factors like frailty may play a significant role.
How can the findings of the RESILIENT-Extend trial be applied to improve stroke care in other low-income populations?
The findings of the RESILIENT-Extend trial offer valuable insights that can be applied to improve stroke care in other low-income populations. One key takeaway is the potential benefit of thrombectomy in the late time window without the need for advanced and costly imaging equipment. This simplified selection criteria based on non-contrast CT imaging can make thrombectomy more accessible and feasible in resource-limited settings. Additionally, the identification of frailty as a factor that correlates with reduced benefit of thrombectomy highlights the importance of considering patient-specific factors in treatment decisions. By tailoring thrombectomy protocols to the specific characteristics of low-income populations, healthcare providers can optimize stroke care outcomes in these settings.
How might the inclusion of frailty as a factor in thrombectomy eligibility criteria impact patient outcomes in different healthcare settings?
The inclusion of frailty as a factor in thrombectomy eligibility criteria can have a significant impact on patient outcomes in different healthcare settings. The RESILIENT-Extend trial observed that older patients in low-income populations, who may be more vulnerable and frail, did not derive the same benefit from thrombectomy as seen in first world countries. This suggests that frailty can act as a ceiling effect for the benefits of thrombectomy, particularly in certain patient populations. By incorporating frailty assessments into thrombectomy eligibility criteria, healthcare providers can better identify patients who are most likely to benefit from the procedure and avoid potential harm in those who may be too frail to withstand the intervention. This personalized approach to treatment selection based on frailty status can lead to improved patient outcomes and more effective utilization of resources in different healthcare settings.
0
