Bone Degradation Measure's Impact on Osteoporosis Diagnosis
Core Concepts
Assessing trabecular bone score (TBS) alongside bone mineral density (BMD) can enhance osteoporosis diagnosis and treatment.
Abstract
Introduction
Assessing bone architecture's key aspect can enhance fracture risk prediction.
TBS is being incorporated alongside BMD for osteoporosis diagnosis.
Impact of TBS
TBS altered diagnosis for 16% of patients at Cleveland Clinic.
TBS helps classify bones as normal, partially degraded, or degraded.
Diagnostic Shifts
Patients' diagnoses shifted based on TBS results.
TBS provides reassurance for patients with thinner bones.
Treatment Implications
TBS aids in prioritizing and tailoring treatment for patients.
TBS helps in obtaining effective therapy for patients.
Reimbursement and Availability
Medicare recently started reimbursing for TBS.
Initial investment in TBS software may be a barrier for health systems.
Potential Drawbacks
TBS software validation limited to specific populations.
Need for broader validation of trabecular bone scoring.
Opportunistic Screening
TBS can be obtained without additional time or radiation.
"Opportunistic screening" for osteoporosis using CT scans.
Bone Quality Assessment
Other aspects of bone quality beyond BMD.
Bone mass remains crucial in assessing bone quality.
Bone Degradation Measure Can Sway Osteoporosis Diagnosis
Stats
"At the Cleveland Clinic Center for Specialized Women's Health in Ohio, factoring in the TBS changed the diagnosis for 16% of 432 patients."
"Among the 432 patients who received a TBS analysis in 2022, 3% shifted from a normal diagnosis to osteopenia, or subclinically low bone density; 8% worsened from osteopenia to osteoporosis; 4% went from osteopenia to normal; and 1.6% downgraded from osteoporosis to osteopenia, Thacker reported."
"More than 600,000 TBS procedures were being performed in the United States each year."
Quotes
"Importantly, 11% got worse diagnoses, and I use that in terms of prioritizing treatment." - Holly Thacker, MD
"When you know that the microarchitecture is normal, you're a lot less concerned that they actually have a bone disease of osteoporosis." - Holly Thacker, MD
"TBS is going to be most helpful in those with osteopenia who are right near the threshold for treatment." - Dr. Marcella Donovan Walker
Key Insights Distilled From
by Jake Remaly at www.medscape.com 10-12-2023
https://www.medscape.com/viewarticle/997324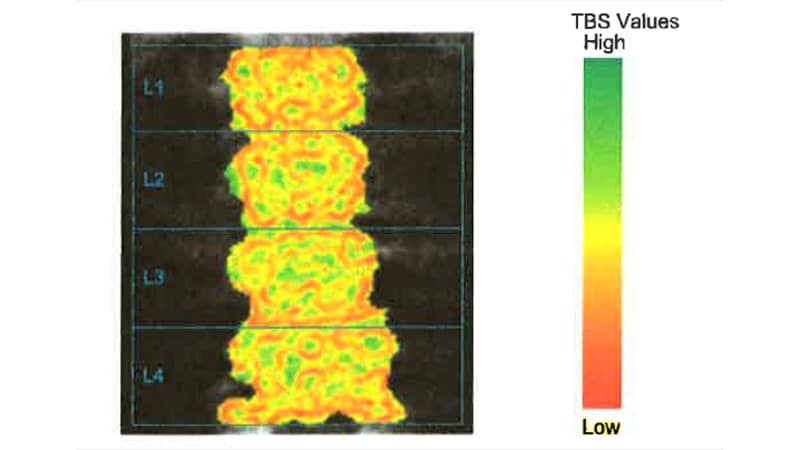
Deeper Inquiries
How can the healthcare system address the financial barriers to implementing TBS for osteoporosis diagnosis and treatment?
The healthcare system can address the financial barriers to implementing TBS for osteoporosis diagnosis and treatment through several strategies. Firstly, advocating for broader insurance coverage and reimbursement for TBS procedures can make it more accessible to patients and healthcare providers. This can involve working with policymakers and insurance companies to recognize the clinical value of TBS and ensure adequate reimbursement rates. Additionally, healthcare systems can explore cost-sharing models where the initial investment in purchasing TBS software is spread across multiple departments or facilities within the system. Collaborating with manufacturers and developers to negotiate lower costs or bulk discounts for TBS software can also help mitigate financial barriers. Furthermore, conducting cost-effectiveness studies to demonstrate the long-term benefits of TBS in preventing fractures and reducing healthcare costs can support the case for investing in this technology.
What are the potential implications of using TBS in populations beyond those it has been validated for?
Using TBS in populations beyond those it has been validated for may have several potential implications. One major concern is the accuracy and reliability of TBS results in diverse populations. If the software has only been validated in specific demographic groups, there is a risk of misdiagnosis or inappropriate treatment recommendations when applied to individuals from different racial or ethnic backgrounds. This could lead to disparities in healthcare outcomes and exacerbate existing health inequities. Additionally, using TBS in unvalidated populations may raise ethical considerations regarding informed consent and patient autonomy. Patients should be informed about the limitations of TBS in their specific demographic group and be involved in shared decision-making regarding their care. Healthcare providers must exercise caution and consider the potential implications of using TBS in populations beyond those it has been validated for to ensure patient safety and quality of care.
How might the incorporation of opportunistic screening for osteoporosis impact overall healthcare practices and patient outcomes?
The incorporation of opportunistic screening for osteoporosis can have significant impacts on overall healthcare practices and patient outcomes. By analyzing existing imaging studies, such as CT scans performed for other purposes, healthcare providers can identify individuals at risk for osteoporosis without the need for additional testing or radiation exposure. This approach can streamline the diagnostic process, leading to earlier detection and intervention for osteoporosis. As a result, patient outcomes may improve, with reduced fracture risk and better management of bone health. Opportunistic screening can also enhance healthcare practices by promoting a more proactive and preventive approach to osteoporosis care. By leveraging existing imaging data to assess bone quality, healthcare providers can optimize resource utilization and prioritize high-risk patients for further evaluation and treatment. Overall, the incorporation of opportunistic screening for osteoporosis has the potential to enhance efficiency, effectiveness, and patient-centered care in healthcare settings.
0
More on Healthcare
