Connective Tissue Disease-Interstitial Lung Disease Discussion
Core Concepts
Understanding and tailoring treatment for CTD-ILD is crucial for patient outcomes.
Abstract
Dr. Swigris introduces the discussion on CTD-ILD, highlighting the importance of understanding the different categories of ILD.
Dr. Danoff shares her personal experience and interest in CTD-ILD, emphasizing the need for attention to underrepresented populations.
The conversation delves into specific categories of ILD, such as RA-ILD, discussing the approach to drug therapy and considerations for treatment.
The discussion extends to systemic autoimmune diseases like SSc-ILD, exploring treatment options like tocilizumab and mycophenolate.
Dr. Danoff provides insights on IPAF, emphasizing the need to tailor therapy based on autoimmune features.
The conversation touches on antisynthetase syndrome in the myositis spectrum, discussing therapy approaches and the role of immunosuppressants.
The experts discuss the role of nintedanib in progressive fibrosis and the importance of shared decision-making in treatment.
Dr. Danoff highlights the significance of seeking expertise from ILD specialty centers and monitoring medication side effects for patient safety.
Episode 1: Connective Tissue Disease-Interstitial Lung Disease
Stats
ILD is categorized into exposures, familial disease, idiopathic causes, and ILD associated with systemic autoimmune disease.
Methotrexate is considered less concerning than TNF inhibitors for ILD treatment.
Patients with RA-ILD may be treated with azathioprine or rituximab.
The INBUILD study showed that patients with progressive fibrotic disease may worsen despite appropriate treatment.
IPAF is a research classification, not a clinical diagnosis.
Tocilizumab has been studied in early active disease but may not be a first-line agent for ILD.
Tacrolimus is effective in patients with MDA-5 antibodies.
IVIG is used in patients with MDA-5 antibodies and rapidly progressive ILDs.
Quotes
"It's never the wrong idea to ask a friend. When you encounter a patient with whom you're really struggling or about whom you're uncertain, refer to an ILD specialty center." - Dr. Danoff
"First, do no harm." - Dr. Danoff
Key Insights Distilled From
by Jeffrey J. S... at www.medscape.com 04-04-2023
https://www.medscape.com/viewarticle/982421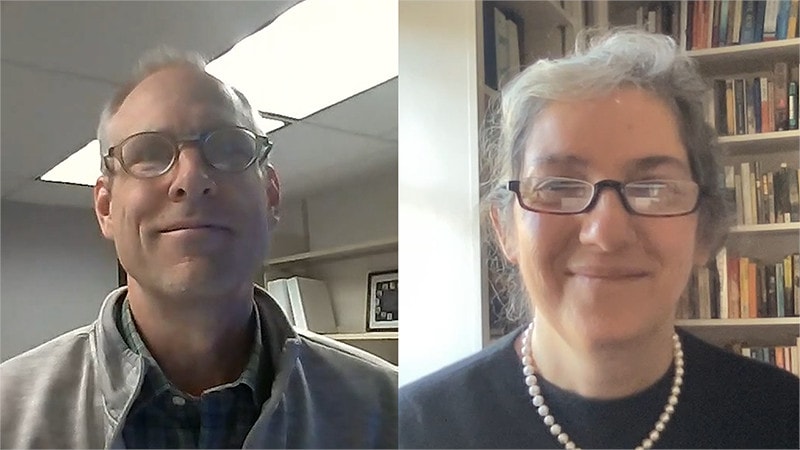
Deeper Inquiries
How can the treatment strategies discussed be adapted for patients in underrepresented populations?
In adapting treatment strategies for underrepresented populations, healthcare providers need to consider cultural factors, language barriers, access to healthcare, and socioeconomic disparities that may impact the management of CTD-ILD. It is crucial to provide culturally competent care, which involves understanding the unique needs and beliefs of patients from different backgrounds. This may include utilizing interpreters, providing educational materials in multiple languages, and being sensitive to cultural preferences in treatment decision-making.
Additionally, healthcare disparities in underrepresented populations may affect access to specialized care and medications. Providers should work to ensure equitable access to treatments, including immunosuppressants and antifibrotics, by addressing financial barriers and collaborating with social workers or patient advocacy groups to navigate insurance coverage and medication assistance programs. Tailoring treatment plans to consider the specific challenges faced by underrepresented populations can improve outcomes and reduce disparities in care.
What are the potential drawbacks of using tocilizumab as a second-line agent for CTD-ILD?
While tocilizumab has shown promise in preserving lung function decline in CTD-ILD, there are potential drawbacks to consider when using it as a second-line agent. One drawback is the lack of long-term data on the efficacy and safety of tocilizumab specifically for CTD-ILD. The drug was initially studied for its effects on skin manifestations in systemic sclerosis, and its impact on lung disease may not be as well-established.
Another drawback is the cost and availability of tocilizumab, which may limit access for some patients. The high cost of biologic therapies like tocilizumab can be a barrier to treatment, especially for underinsured or uninsured individuals. Additionally, the side effect profile of tocilizumab, including the risk of infections and infusion reactions, should be carefully considered when choosing it as a second-line agent.
Furthermore, the optimal timing and patient selection for tocilizumab in CTD-ILD remain areas of ongoing research and debate. Without clear guidelines on when to introduce tocilizumab in the treatment algorithm and which patients are most likely to benefit, there is a risk of suboptimal outcomes or unnecessary exposure to potential risks.
How can advancements in understanding IPAF impact the diagnosis and treatment of ILD in the future?
Advancements in understanding IPAF have the potential to significantly impact the diagnosis and treatment of ILD in the future by improving the recognition of autoimmune features in patients with interstitial pneumonia. As research continues to refine the criteria and classification of IPAF, clinicians will be better equipped to identify patients who may benefit from early immunosuppressive therapy based on autoimmune features present in their ILD.
Improved understanding of IPAF can lead to more personalized and targeted treatment approaches for patients with ILD, especially those who do not fit neatly into existing diagnostic categories like idiopathic pulmonary fibrosis or connective tissue disease-associated ILD. By recognizing and addressing autoimmune features in ILD, clinicians can tailor therapy to target the underlying inflammatory processes driving lung fibrosis, potentially leading to better outcomes and disease management.
Furthermore, advancements in IPAF research may contribute to the development of novel therapeutic strategies that specifically target autoimmune mechanisms implicated in the pathogenesis of ILD. By elucidating the immune pathways involved in IPAF-related lung disease, researchers can identify new drug targets and treatment modalities that address the unique immunological aspects of these conditions. This could pave the way for more effective and individualized therapies for patients with ILD, ultimately improving their quality of life and prognosis.
0
