Factors to Consider When Deprescribing Hypertension Drugs
Core Concepts
Knowing when to deprescribe blood pressure medications is crucial for patient comfort and quality of life.
Abstract
Eugene Yang, MD, emphasizes the importance of considering age, comorbidities, and functional status when deciding to deprescribe hypertension drugs. Guidelines for hypertension management vary between regions, with a focus on individualized treatment plans. Research suggests that reducing hypertensive medication may not lead to significant blood pressure fluctuations. Tailored approaches are necessary for patients with comorbidities, with lifestyle changes recommended as the first step for grade 1 hypertension. Continuous medication is crucial for patients with heart failure to prevent further deterioration. Careful monitoring and gradual dose reduction are essential when deprescribing certain medications.
Factors to Consider When Deprescribing Hypertension Drugs
Stats
Hypertension was a primary or contributing cause of nearly 700,000 deaths in the United States in 2021.
Nearly half of adults in the US have hypertension, but only about one in four have it under control.
The mean age of participants in a study on reducing hypertensive medication was 66 years.
Quotes
"In a patient where we have a limited life expectancy, where they have limited function or core memory, the goal is not to prolong life: It's to make them more comfortable." - Eugene Yang, MD
Key Insights Distilled From
by Lindsay Kalt... at www.medscape.com 02-15-2024
https://www.medscape.com/viewarticle/rethinking-hypertension-care-evolving-landscape-2024a1000383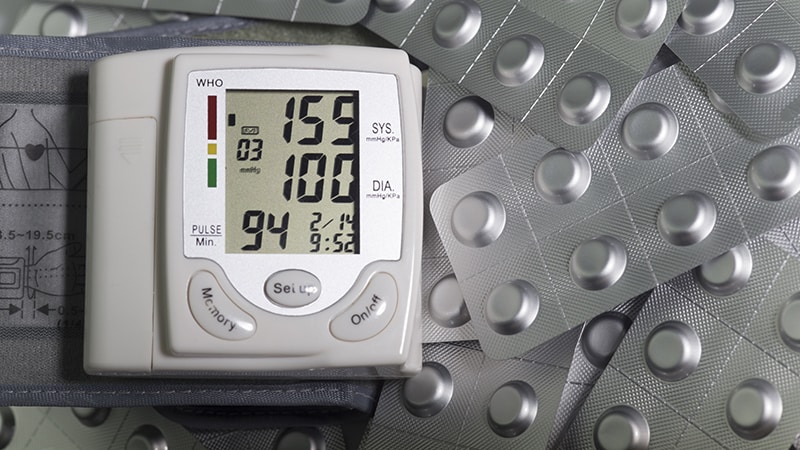
Deeper Inquiries
How can guidelines for hypertension management be standardized across different regions?
Standardizing guidelines for hypertension management across different regions requires collaboration among international medical organizations to establish universal protocols. This can involve creating a consensus on diagnostic criteria, treatment thresholds, and medication recommendations. By aligning these guidelines, healthcare providers worldwide can follow a cohesive approach to managing hypertension, ensuring consistency in care delivery and improving patient outcomes. Additionally, ongoing communication and knowledge-sharing between healthcare professionals globally can help disseminate best practices and facilitate the adoption of standardized guidelines across diverse healthcare systems.
What are the potential risks of reducing hypertensive medication too quickly?
Reducing hypertensive medication too quickly can pose several risks to patients, including rebound hypertension, where blood pressure spikes to dangerous levels. Abrupt withdrawal of certain medications, such as central-acting medications like clonidine and beta-blockers, can lead to adverse effects due to the sudden alteration in cardiovascular function. Patients may experience symptoms like palpitations, dizziness, headaches, and even cardiovascular events like heart attacks or strokes. Therefore, a gradual tapering of medication under close medical supervision is essential to prevent these risks and ensure a safe transition in hypertension management.
How can patient empowerment through self-monitoring improve hypertension management outcomes?
Patient empowerment through self-monitoring plays a crucial role in improving hypertension management outcomes by promoting active patient engagement and early detection of blood pressure fluctuations. By teaching patients how to monitor their blood pressure at home using accurate techniques, healthcare providers empower individuals to take charge of their health and track their progress regularly. This self-monitoring approach enables patients to identify any deviations from their baseline readings promptly, allowing for timely intervention and adjustment of treatment plans. Moreover, self-monitoring fosters a sense of ownership and responsibility for one's health, leading to better adherence to medication regimens, lifestyle modifications, and follow-up appointments, ultimately enhancing hypertension management outcomes.
0
More on Healthcare
