Improved Early Detection of Ovarian Cancer in Postmenopausal Women
Core Concepts
Early detection of ovarian cancer in postmenopausal women is crucial for improving outcomes.
Abstract
Standalone Note here
TOPLINE:
- Two-step screening strategy in postmenopausal women showed high specificity, sensitivity, and positive predictive value for ovarian and borderline cancer.
- Most cancers detected were at stage I or II.
METHODOLOGY:
- Early detection at stage I or II can reduce ovarian cancer-related deaths significantly.
- 7856 postmenopausal women underwent annual ovarian cancer screening from 2011 to 2022.
- Screening involved annual blood tests for cancer antigen 125 levels.
- Risk of Ovarian Cancer Algorithm (ROCA) used to assess cancer risk.
- Elevated ROCA scores led to transvaginal sonography or follow-up blood tests.
TAKEAWAY:
- 95.5% of women referred for ultrasound had one.
- 50% of patients with suspicious findings had ovarian cancer.
- 74% of patients with abnormal ROCA results had any cancer.
- Specificity for ultrasound was 98%, and for surgery was 99.8%.
- Sensitivity for detecting ovarian and borderline cancer was 74%.
IN PRACTICE:
- 70% of ovarian cancers detected were early stage.
- High specificity and positive predictive value support further development of this strategy.
LIMITATIONS:
- Trial not powered to detect mortality benefit.
- Six cancers and borderline tumors were missed.
- Sensitivity may be limited by the fact that only 80% of ovarian cancers express cancer antigen 125.
SOURCE:
- Study led by Chae Young Han from the University of Texas MD Anderson Cancer Center, published in the Journal of Clinical Oncology.
DISCLOSURES:
- Study supported by various organizations, with authors receiving research funding, grants, and fees from multiple companies.
Customize Summary
Rewrite with AI
Generate Citations
Translate Source
To Another Language
Generate MindMap
from source content
Visit Source
www.medscape.com
New Strategy Improves Early-Stage Ovarian Cancer Detection
Stats
"Detecting ovarian cancer at stage I or II could significantly reduce ovarian cancer-related deaths, but only 25%-30% of patients are diagnosed at an early stage."
"Overall, 92.3% of women were normal risk, 5.7% were intermediate, and 2% were high risk and recommended for transvaginal sonography."
"Of 34 patients with suspicious findings and recommended for surgery, 15 had ovarian cancer and two had borderline tumors, indicating a positive predictive value of 50% (17 of 34 patients) for ovarian cancer."
"The specificity for elevated risk ROCA prompting ultrasound was 98%, and the specificity of the ROCA and ultrasound prompting surgery was 99.8%."
"The sensitivity for detecting ovarian and borderline cancer was 74% (17 of 23)."
Quotes
"Remarkably, 70% of ovarian cancers detected by the ROCA" were early stage."
"Although the trial was not powered to detect reduced mortality, the high specificity, positive predictive value, and shift to identifying earlier-stage cancers support further development of this strategy."
Key Insights Distilled From
by Deepa Varma at www.medscape.com 01-25-2024
https://www.medscape.com/viewarticle/two-step-strategy-improves-early-stage-ovarian-cancer-2024a10001sq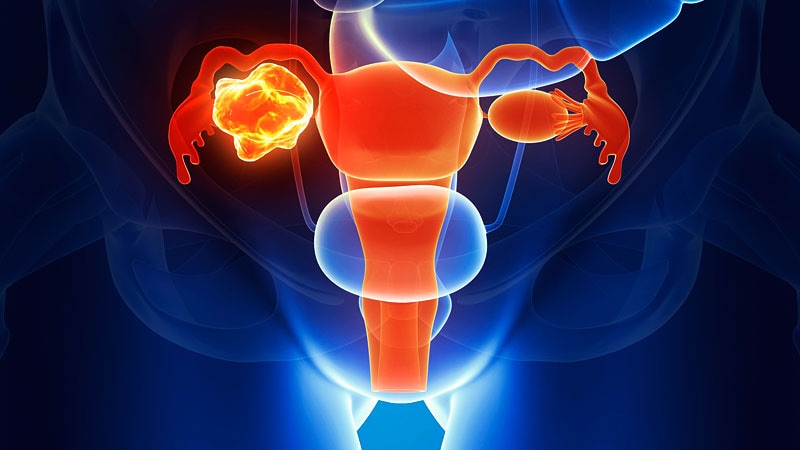
Deeper Inquiries
How can this two-step screening strategy be implemented on a larger scale to benefit more women?
To implement this two-step screening strategy on a larger scale and benefit more women, several key steps can be taken. Firstly, raising awareness among healthcare providers and the general public about the importance of early detection of ovarian cancer is crucial. This can be achieved through educational campaigns, workshops, and collaborations with medical organizations. Additionally, integrating this screening strategy into routine healthcare check-ups for postmenopausal women can help reach a larger population. Establishing partnerships with healthcare facilities and insurance providers to cover the costs of screening can also make it more accessible to a broader demographic. Furthermore, leveraging telemedicine and digital health platforms can facilitate remote screening and monitoring, making it easier for women in rural or underserved areas to participate in the screening program.
What are the potential drawbacks or risks associated with relying heavily on the ROCA algorithm for cancer detection?
While the ROCA algorithm has shown promising results in detecting ovarian cancer at early stages, there are potential drawbacks and risks associated with relying heavily on this method for cancer detection. One limitation is the false-positive rate, which may lead to unnecessary anxiety, additional testing, and potential overtreatment for patients. Moreover, the algorithm's sensitivity may not be sufficient to detect all cases of ovarian cancer, especially in individuals whose tumors do not express the cancer antigen 125. Depending solely on the ROCA algorithm may also overlook other types of cancers or health conditions that present with similar biomarker patterns, leading to misdiagnosis or delayed treatment. Additionally, the cost of implementing and maintaining the ROCA screening program on a large scale could be a barrier for widespread adoption, potentially limiting access for certain populations.
How can advancements in technology further improve the accuracy and efficiency of early-stage cancer detection methods?
Advancements in technology hold great potential to enhance the accuracy and efficiency of early-stage cancer detection methods. One key area of improvement is the development of more sensitive and specific biomarkers that can detect a wider range of cancer types at earlier stages. Utilizing artificial intelligence and machine learning algorithms to analyze complex datasets, including genetic, imaging, and clinical information, can help identify patterns and markers that may not be apparent to human observers. Incorporating liquid biopsy techniques that analyze circulating tumor cells, DNA, and RNA in the blood can provide a less invasive and more real-time approach to monitoring cancer progression. Furthermore, the integration of wearable devices and remote monitoring tools can enable continuous tracking of biomarkers and symptoms, allowing for early intervention and personalized treatment plans. Collaborations between researchers, clinicians, and technology experts are essential to drive innovation in early-stage cancer detection and improve patient outcomes.
0
