Liquid Biopsy Impact on NSCLC Treatment Time
Core Concepts
Adding plasma ctDNA testing before tissue biopsy can significantly reduce time to treatment for advanced NSCLC patients.
Abstract
The study explores the impact of liquid biopsy with next-generation sequencing (NGS) on the time to treatment for patients with advanced non–small cell lung cancer (NSCLC). Here are the key highlights and insights:
- Liquid biopsy with NGS and standard tissue biopsy reduced time to treatment by 23 days.
- 23% of patients started targeted therapy based on plasma ctDNA findings alone.
- Median time to treatment for patients diagnosed with advanced NSCLC in the liquid biopsy group was 27 days.
- The study suggests the clinical utility of adding plasma ctDNA testing before tissue biopsy for suspected advanced lung cancer.
- Molecular testing of tumor tissue remains the standard for diagnosing NSCLC.
- Liquid biopsy complements tissue biopsy for advanced NSCLC.
- The median time to treatment was significantly shorter for the liquid biopsy group compared to the reference cohort.
- Complementing standard tissue testing with plasma testing could increase access to precision medicine.
- Time to treatment is crucial, especially for patients with aggressive NSCLC histology.
- Liquid biopsy sensitivity continues to improve, but tissue biopsy remains essential for diagnosis and subtyping.
Customize Summary
Rewrite with AI
Generate Citations
Translate Source
To Another Language
Generate MindMap
from source content
Visit Source
www.medscape.com
Liquid Biopsy Shortens Time to NSCLC Treatment
Stats
Patients who underwent liquid biopsy with NGS and standard tissue biopsy received treatment within a median of 39 days, vs 62 days for those diagnosed through standard tissue biopsy alone.
Of the 90 patients diagnosed with advanced NSCLC in the liquid biopsy group, 23% started targeted therapy on the basis of their plasma ctDNA findings alone; the median time to treatment was 27 days.
The median turnaround time from plasma sample collection to genotyping results was 7 days for the liquid biopsy group, vs 23 days for tissue NGS.
Quotes
"The last thing you want, in this era where you have nine different targeted therapies for lung cancer, is to give the wrong drug to the wrong patient or to give them chemotherapy or immunotherapy when they have a targetable abnormality." - Roy S. Herbst, MD, PhD
"With EGFR mutations, within 3 weeks or even days, sometimes you'll see patients starting to present with symptoms, so time does matter." - Roy S. Herbst, MD, PhD
Key Insights Distilled From
by Neil Osterwe... at www.medscape.com 08-04-2023
https://www.medscape.com/viewarticle/995169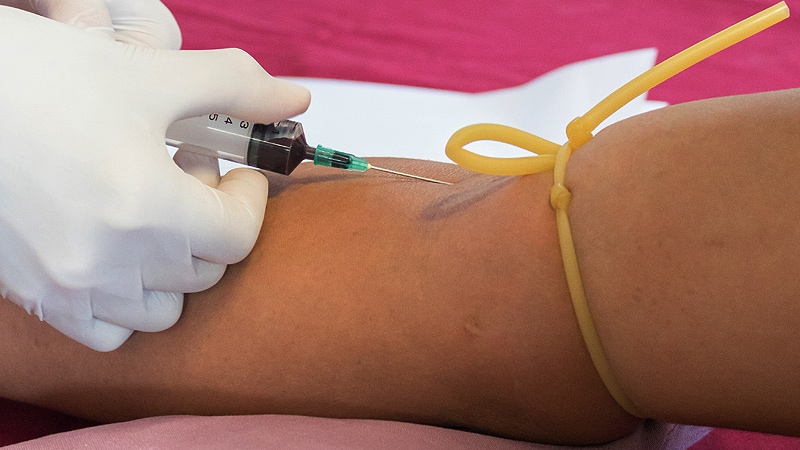
Deeper Inquiries
How can the integration of liquid biopsy and tissue biopsy be optimized to enhance patient outcomes?
The integration of liquid biopsy and tissue biopsy can be optimized by establishing clear guidelines and protocols for when each type of biopsy should be used. For example, using liquid biopsy as a first-line screening tool to identify potential mutations quickly, followed by confirmation through tissue biopsy for accurate diagnosis. This sequential approach can help expedite the diagnostic process and ensure that patients receive appropriate treatment in a timely manner. Additionally, healthcare providers should be educated on the benefits of combining both biopsy methods and the importance of interpreting results in conjunction to make informed treatment decisions. Collaboration between oncologists, pathologists, and other specialists is crucial to ensure seamless integration and coordination of care for patients.
What are the potential drawbacks or limitations of relying on liquid biopsy alone for diagnosing NSCLC?
Relying on liquid biopsy alone for diagnosing NSCLC has several potential drawbacks and limitations. One major limitation is the sensitivity and specificity of liquid biopsy compared to tissue biopsy. While liquid biopsy can provide valuable information about tumor mutations, it may not always capture the full genetic profile of the tumor, leading to potential false-negative results or missing important mutations. Additionally, the technology and techniques used in liquid biopsy are still evolving, which can impact the accuracy and reliability of the results. Another limitation is the need for confirmation through tissue biopsy in cases where liquid biopsy results are inconclusive or contradictory. Without tissue biopsy, there is a risk of misdiagnosis or inappropriate treatment selection based on incomplete information. Therefore, while liquid biopsy can be a valuable tool in the diagnostic process, it should be used in conjunction with tissue biopsy to ensure comprehensive and accurate diagnosis.
How can the healthcare system adapt to incorporate advanced diagnostic technologies like liquid biopsy effectively?
To incorporate advanced diagnostic technologies like liquid biopsy effectively, the healthcare system needs to invest in infrastructure, training, and resources to support the implementation of these technologies. This includes providing education and training for healthcare providers on how to collect, analyze, and interpret liquid biopsy results accurately. Additionally, guidelines and protocols should be developed to standardize the use of liquid biopsy in clinical practice and ensure consistency in testing and reporting. Collaboration between healthcare institutions, research organizations, and industry partners is essential to drive innovation and advancements in liquid biopsy technology. Furthermore, reimbursement policies and insurance coverage should be updated to support the use of liquid biopsy as a diagnostic tool, ensuring that patients have access to these cutting-edge technologies without financial barriers. By fostering a supportive environment for the adoption of advanced diagnostic technologies, the healthcare system can improve patient outcomes and enhance the quality of care provided to individuals with NSCLC.
0
