Polygenic Risk Score Testing for Prostate Cancer Risk Assessment
Core Concepts
Polygenic risk score testing shows promise in predicting prostate cancer risk but faces challenges in clinical utility.
Abstract
Standalone Note here
DNA Testing for Prostate Cancer
DNA testing used in the US for low-grade, localized prostate cancers.
Polygenic Risk Score (PRS)
PRS emerging as a genetic approach for prostate cancer risk.
Integrates common variants to estimate disease risk.
Utility of PRS
PRS can predict prostate cancer risk but struggles to differentiate aggressive vs nonaggressive disease.
Research and Findings
Genome-wide studies lead to better PRS development.
Largest prostate GWAS analysis identified new genetic risk variants.
Challenges and Criticisms
Studies show limitations in predicting aggressive prostate cancers.
Concerns over PRS communication and clinical utility.
Future Implications
PRS could guide treatment choices and inform cancer screening.
Infrastructure for PRS testing in the US is lacking.
Predicting Prostate Cancer Risk: Is PRS Testing Ready?
Stats
"Compared with men at average genetic risk for prostate cancer — those in the 40% to 60% genetic risk score category — men in the top 10% of the risk score (90% to 100%) had between a 3.74-fold to fivefold higher risk for prostate cancer."
"About 40% of men who will develop aggressive disease have a PRS in the top 20%, whereas only about 7% of men who will develop aggressive tumors have a PRS in the bottom 20%."
"Men in the top 20% of the PRS distribution had an almost three times higher risk of prostate cancer compared with men in the lowest quintile."
Quotes
"While a PRS for prostate cancer is strongly associated with incident risk, the clinical utility of the PRS as a biomarker is currently limited by its inability to select for clinically significant disease."
"Risk is notoriously difficult to communicate."
Key Insights Distilled From
by Howard Wolin... at www.medscape.com 09-05-2023
https://www.medscape.com/viewarticle/996114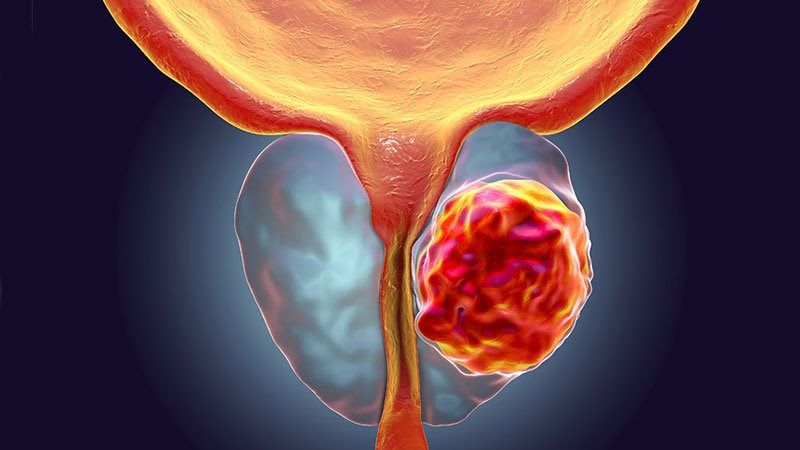
Deeper Inquiries
How can the limitations of PRS in predicting aggressive prostate cancers be addressed?
While PRS has shown promise in predicting overall prostate cancer risk, its limitations in distinguishing between aggressive and nonaggressive disease remain a challenge. To address this issue, further research is needed to refine the PRS by incorporating additional genetic markers that specifically correlate with aggressive prostate cancer. By identifying and validating these markers through large-scale studies, the predictive accuracy of PRS for aggressive disease can be improved. Additionally, integrating other clinical parameters such as PSA levels, imaging results, and family history into the PRS model may enhance its ability to stratify patients based on the aggressiveness of their prostate cancer. Collaborative efforts among researchers, clinicians, and geneticists are essential to overcome the current limitations of PRS in predicting aggressive prostate cancers.
What are the ethical implications of using PRS to inform cancer screenings?
The use of PRS to inform cancer screenings raises several ethical considerations that need to be carefully addressed. One major concern is the potential for overdiagnosis and overtreatment of individuals with high-risk PRS scores. Patients with elevated PRS may undergo unnecessary invasive procedures or treatments based solely on their genetic risk, leading to physical, emotional, and financial burdens. Moreover, there is a risk of genetic determinism, where individuals may feel fatalistic about their health outcomes based on their PRS results, potentially impacting their mental well-being. Additionally, disparities in access to PRS testing and subsequent screenings could exacerbate existing healthcare inequities, as certain populations may face barriers to obtaining and interpreting their genetic risk information. Healthcare providers must ensure that patients receive comprehensive genetic counseling and education about the limitations of PRS, empowering them to make informed decisions about cancer screenings based on their individual circumstances.
How can the healthcare system adapt to incorporate PRS testing for better patient outcomes?
To effectively integrate PRS testing into routine clinical practice and improve patient outcomes, the healthcare system must undergo several adaptations. Firstly, healthcare providers need to receive training and education on how to interpret and communicate PRS results to patients in a clear and understandable manner. Genetic counselors play a crucial role in helping individuals navigate the complexities of genetic risk information and make informed decisions about their healthcare. Secondly, electronic health records should be updated to include PRS data, allowing clinicians to easily access and utilize this information during patient consultations. Collaborative efforts between geneticists, oncologists, primary care physicians, and other healthcare professionals are essential to establish guidelines for incorporating PRS into cancer screening protocols. Additionally, insurance coverage for PRS testing needs to be expanded to ensure equitable access for all patients, regardless of their socioeconomic status. By fostering multidisciplinary collaboration, enhancing provider education, and improving infrastructure support, the healthcare system can effectively leverage PRS testing to personalize cancer screening strategies and ultimately enhance patient outcomes.
0
More on Healthcare
