The Reality of Fertility Technology: IVF and Future Innovations
Core Concepts
Advancements in fertility technology, such as AI, robotics, genetic testing, and stem cells, are revolutionizing IVF treatments and offering hope to millions struggling with infertility.
Abstract
Introduction
- Personal journey of IVF after multiple losses.
- Global infertility statistics and rising demand for assisted reproductive technology.
Current Challenges in Fertility Treatments
- Limited clinician availability and high costs.
- Need for a million-plus IVF cycles to meet demand.
Role of Technology in Fertility Treatments
- AI assisting in decision-making and embryo grading.
- Use of robots in IVF labs for precise and repetitive tasks.
Innovations in Genetic Testing
- Development of STORK test for genetic testing without embryo freezing.
- Cost and time-saving benefits for couples undergoing genetic testing.
Simplifying Sperm Collection
- Introduction of at-home sperm collection boxes.
- Increased comfort and success rates for patients.
Wearable Devices for Reproductive Health
- Tempdrop, Bellabeat Ivy, and Mirvie aiding in fertility tracking.
- Move towards at-home monitoring for streamlined processes.
Stem Cells and Future Possibilities
- Research on creating eggs and sperm from stem cells.
- Potential game-changer in fertility treatments.
Customize Summary
Rewrite with AI
Generate Citations
Translate Source
To Another Language
Generate MindMap
from source content
Visit Source
www.medscape.com
The Fertile Future of Fertility Technology
Stats
Global estimates: 48 million couples and 186 million individuals struggle with infertility.
Average cost of an IVF cycle: $23,500.
2 million infants born in the US each year through assisted reproductive technology.
1250 practicing fertility physicians in the US.
250,000 to 300,000 IVF cycles performed annually in the US.
Quotes
"The field is really coming into an age of great progress and innovation." - Zev Williams, MD, PhD
"Rather than me making decisions from a couple of thousands of cycles of experience, I get to leverage hundreds of thousands of cycles from different providers over different people." - Eduardo Hariton, MD
"It's a win-win because you allow the robots to do things better than a human can and this allows the humans to do things that a robot just can't do." - Zev Williams, MD, PhD
Key Insights Distilled From
by Nicole Pajer at www.medscape.com 07-27-2023
https://www.medscape.com/viewarticle/994894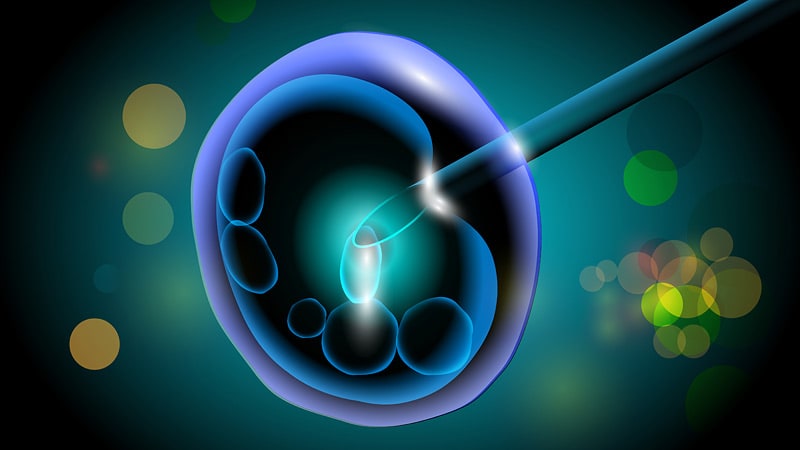
Deeper Inquiries
How can the integration of AI and robotics in fertility treatments impact the patient experience and success rates?
The integration of AI and robotics in fertility treatments can have a significant impact on both the patient experience and success rates. AI can assist in decision-making processes by analyzing vast amounts of data from different providers to make objective decisions about the optimal treatment for each patient. This can lead to more personalized and effective treatment plans, ultimately improving success rates. Additionally, AI can help with tasks like embryo grading, ensuring the selection of the best embryo for transfer.
On the other hand, robotics, such as articulated (ART) robots, can handle precise and repetitive tasks in the IVF lab, such as creating special plates for embryo growth. By automating these processes, robots can improve efficiency and accuracy, leading to better outcomes. For example, the use of robots in sperm collection can provide a more comfortable experience for patients and increase the success rate of collected samples.
Overall, the integration of AI and robotics in fertility treatments can streamline processes, enhance precision, and optimize decision-making, ultimately improving the patient experience and increasing success rates in assisted reproductive technology.
How might wearable devices and at-home monitoring transform the future of reproductive healthcare beyond fertility treatments?
Wearable devices and at-home monitoring have the potential to transform the future of reproductive healthcare beyond fertility treatments by providing individuals with greater control over their reproductive health. These devices, such as the Tempdrop Fertility and Ovulation Tracker and the Bellabeat Ivy smart bracelet, can help women track their menstrual cycles, ovulation, and fertility more accurately. By harnessing biometric data, these wearables can predict periods, ovulation, and fertility, empowering individuals to make informed decisions about their reproductive health.
At-home monitoring devices also offer privacy and convenience, allowing patients to monitor their reproductive health from the comfort of their homes. For example, remote ultrasounds and at-home hormone monitors like Mira enable patients to access essential reproductive health services without frequent visits to healthcare facilities. This not only improves accessibility but also promotes early detection of reproductive health issues.
Furthermore, advancements in at-home monitoring can extend beyond fertility treatments to include pregnancy monitoring, postnatal care, and even predicting pregnancy complications. For instance, the development of Mirvie, a blood test that can predict pregnancy complications earlier, showcases the potential of at-home monitoring to revolutionize reproductive healthcare by providing timely and accurate insights into reproductive health beyond fertility treatments.
What ethical considerations should be taken into account when utilizing stem cells for creating eggs and sperm?
When utilizing stem cells for creating eggs and sperm, several ethical considerations must be taken into account to ensure responsible and ethical practices in reproductive healthcare. One of the primary ethical concerns is the source of stem cells, as obtaining stem cells from embryos or other controversial sources raises ethical dilemmas regarding the destruction of embryos and the potential for exploitation.
Additionally, the use of stem cells for reproductive purposes raises questions about the safety and long-term implications of such technologies. Ensuring the safety and efficacy of stem cell-based treatments is crucial to protect the well-being of patients and offspring conceived through these methods.
Furthermore, issues related to consent, privacy, and genetic manipulation must be carefully addressed when utilizing stem cells for creating eggs and sperm. Patients should be fully informed about the procedures, risks, and potential outcomes of using stem cell-based technologies in reproductive healthcare. Respect for patient autonomy, confidentiality, and genetic integrity is essential in navigating the ethical complexities of stem cell-based reproductive technologies.
Overall, a comprehensive ethical framework that considers the source of stem cells, safety concerns, patient consent, and genetic implications is essential to guide the responsible and ethical use of stem cells for creating eggs and sperm in reproductive healthcare.
0
