insight - Immunology - # Tumor-infiltrating stem-like CD8+ T cells and the immunosuppressive role of prostaglandin E2
Prostaglandin E2 Suppresses Expansion and Effector Differentiation of Tumor-Infiltrating Stem-like CD8+ T Cells
Core Concepts
Tumor-derived prostaglandin E2 (PGE2) restricts the proliferative expansion and effector differentiation of TCF1+ stem-like CD8+ T cells within tumors, promoting cancer immune escape.
Abstract
The article investigates the mechanisms that limit the anticancer immunity mediated by tumor-infiltrating stem-like CD8+ T cells (TCF1+ CD8+ T cells). The key findings are:
Tumor-derived PGE2 does not affect the priming of TCF1+ CD8+ T cells in draining lymph nodes, but it restricts their proliferative expansion and effector differentiation within the tumor microenvironment.
PGE2 acts through EP2 and EP4 (EP2/EP4) receptor signaling in CD8+ T cells to limit the intratumoral generation of early and late effector T cell populations that originate from TCF1+ tumor-infiltrating CD8+ T lymphocytes (TILs).
Ablation of EP2/EP4 signaling in cancer-specific CD8+ T cells rescues their expansion and effector differentiation within tumors, leading to tumor elimination in multiple mouse cancer models.
The suppression of the interleukin-2 (IL-2) signaling pathway underlies the PGE2-mediated inhibition of TCF1+ TIL responses.
The study identifies the PGE2–EP2/EP4 axis as a molecular target to restore IL-2 responsiveness in anticancer TILs and achieve cancer immune control.
PGE2 limits effector expansion of tumour-infiltrating stem-like CD8+ T cells - Nature
Stats
Tumor-derived prostaglandin E2 (PGE2) restricts the proliferative expansion and effector differentiation of TCF1+ stem-like CD8+ T cells within tumors.
Ablation of EP2/EP4 signaling in cancer-specific CD8+ T cells rescues their expansion and effector differentiation within tumors, leading to tumor elimination in multiple mouse cancer models.
Quotes
"PGE2 acts through EP2 and EP4 (EP2/EP4) receptor signalling in CD8+ T cells to limit the intratumoural generation of early and late effector T cell populations that originate from TCF1+ tumour-infiltrating CD8+ T lymphocytes (TILs)."
"Suppression of the interleukin-2 (IL-2) signalling pathway underlies the PGE2-mediated inhibition of TCF1+ TIL responses."
Key Insights Distilled From
by Seba... at www.nature.com 04-24-2024
https://www.nature.com/articles/s41586-024-07254-x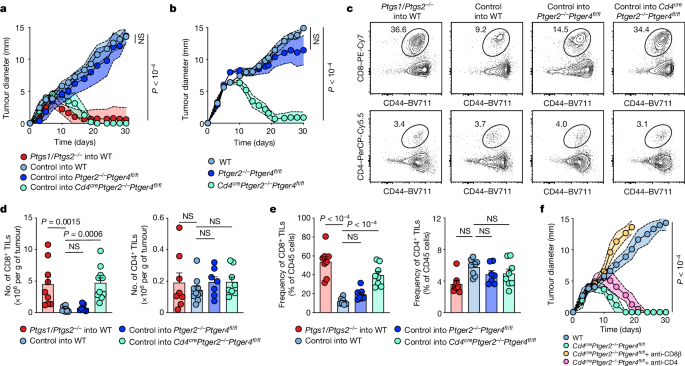
Deeper Inquiries
How could the PGE2–EP2/EP4 axis be targeted therapeutically to enhance the anticancer activity of TCF1+ stem-like CD8+ T cells in human cancers?
The PGE2–EP2/EP4 axis can be targeted therapeutically to enhance the anticancer activity of TCF1+ stem-like CD8+ T cells in human cancers by developing specific inhibitors or antagonists that block the interaction between PGE2 and its receptors EP2 and EP4. By inhibiting this signaling pathway, the suppressive effects of PGE2 on the expansion and effector differentiation of TCF1+CD8+ T cells within the tumor microenvironment can be alleviated, allowing for enhanced anticancer immune responses. Additionally, strategies such as using EP2/EP4 receptor antagonists or blocking downstream signaling pathways activated by EP2/EP4 could be explored to restore the IL-2 responsiveness of TCF1+ TILs and promote their effector functions against cancer cells.
What other immunosuppressive mechanisms, besides the PGE2–EP2/EP4 axis, might be involved in limiting the expansion and effector differentiation of TCF1+ stem-like CD8+ T cells within the tumor microenvironment?
Apart from the PGE2–EP2/EP4 axis, other immunosuppressive mechanisms that might be involved in limiting the expansion and effector differentiation of TCF1+ stem-like CD8+ T cells within the tumor microenvironment include the upregulation of inhibitory receptors such as PD-1, CTLA-4, and TIM-3, which can inhibit T cell activation and effector functions. The presence of immunosuppressive cells like regulatory T cells (Tregs) and myeloid-derived suppressor cells (MDSCs) in the tumor microenvironment can also contribute to the suppression of TCF1+CD8+ T cell responses. Additionally, metabolic factors such as nutrient deprivation, hypoxia, and the accumulation of metabolites like adenosine can create an immunosuppressive microenvironment that hinders the function of TCF1+ stem-like CD8+ T cells.
Given the importance of IL-2 signaling in regulating TCF1+ stem-like CD8+ T cell responses, what other metabolic or signaling pathways could be targeted to boost the antitumor function of these cells?
In addition to targeting the IL-2 signaling pathway, other metabolic or signaling pathways that could be targeted to boost the antitumor function of TCF1+ stem-like CD8+ T cells include the mTOR pathway, which plays a crucial role in T cell activation and effector functions. By modulating mTOR signaling, either through inhibitors like rapamycin or activators like IL-15, the effector differentiation and cytotoxic activity of TCF1+CD8+ T cells can be enhanced. Furthermore, targeting metabolic pathways such as glycolysis, fatty acid oxidation, and amino acid metabolism can provide metabolic support to TCF1+ TILs, improving their survival and function within the tumor microenvironment. Strategies that promote mitochondrial fitness and biogenesis in TCF1+CD8+ T cells can also enhance their antitumor responses by increasing their energy production and effector capabilities.
0
