The Importance of Biomarker Testing in Gastroesophageal Cancer Treatment
Core Concepts
Improving biomarker testing is crucial for optimizing treatment outcomes in gastroesophageal cancer.
Abstract
The article emphasizes the significance of biomarker testing in the treatment of advanced gastroesophageal cancer. Dr. Yelena Janjigian highlights the importance of routine testing for biomarkers to enhance patient outcomes. Key biomarkers such as MSI, HER2, and PD-L1 are discussed, along with the impact of targeted therapies on survival rates. The need for continued advancements in patient selection through biomarker testing is underscored.
Customize Summary
Rewrite with AI
Generate Citations
Translate Source
To Another Language
Generate MindMap
from source content
Visit Source
www.medscape.com
The Case for Biomarker Testing in Gastroesophageal Cancer
Stats
Only about 40% of patients undergo biomarker testing.
Median overall survival for patients with high MSI who received nivolumab plus chemotherapy was 38.7 months.
Patients with a PD-L1 CPS of 5 or higher had a significantly higher median overall survival of 14.4 months.
Median overall survival in HER2-positive patients with a PD-L1 CPS of 1 or more was 20.0 months.
Quotes
"Biomarker testing needs to improve to ensure patients benefit from targeted therapies."
"We need to be smarter about patient selection by using biomarker testing."
Key Insights Distilled From
by M. Alexander... at www.medscape.com 01-22-2024
https://www.medscape.com/viewarticle/case-biomarker-testing-gastroesophageal-cancer-2024a10001ko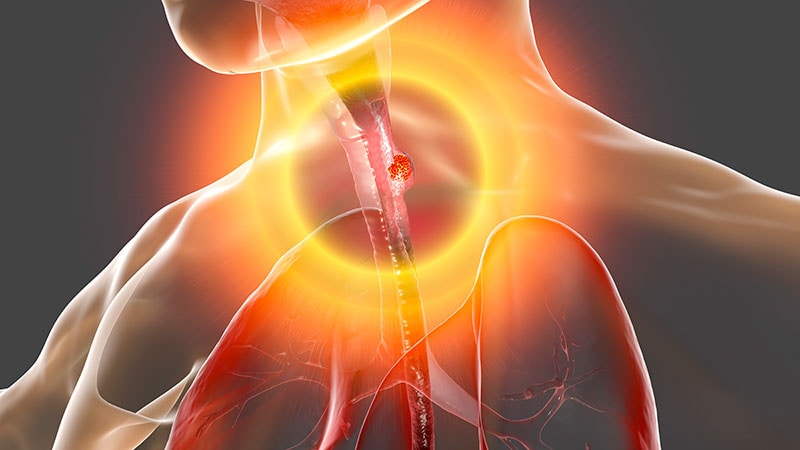
Deeper Inquiries
How can healthcare systems improve access to biomarker testing for gastroesophageal cancer patients?
Healthcare systems can improve access to biomarker testing for gastroesophageal cancer patients by implementing standardized protocols that prioritize testing for key biomarkers like Microsatellite instability (MSI), human epidermal growth factor receptor 2 (HER2), and programmed death–ligand 1 (PD-L1). This can involve integrating biomarker testing into routine clinical practice guidelines, ensuring that testing is readily available, and providing training for healthcare staff to facilitate the testing process. Additionally, leveraging technology and telemedicine can help reach patients in remote areas who may have limited access to testing facilities.
What challenges exist in implementing routine biomarker testing in clinical practice?
Several challenges exist in implementing routine biomarker testing in clinical practice, including inertia and logistical barriers, lack of awareness among healthcare providers, limited resources, and variability in testing methodologies. In some cases, there may be resistance to change traditional treatment approaches, and the cost of testing can also be a barrier. Furthermore, interpreting and acting upon the results of biomarker testing require specialized knowledge and expertise, which may not always be readily available in all healthcare settings.
How can advancements in biomarker testing impact treatment outcomes in other types of cancer?
Advancements in biomarker testing can have a significant impact on treatment outcomes in other types of cancer by enabling personalized and targeted therapies. By identifying specific biomarkers associated with certain cancers, healthcare providers can tailor treatment plans to individual patients, increasing the likelihood of treatment success and reducing the risk of adverse effects. Additionally, biomarker testing can help predict response to certain therapies, allowing for more effective treatment selection and monitoring. As more biomarkers are discovered and validated, the potential for improving treatment outcomes across various types of cancer continues to grow.
0
