Genomic Evolution of Small Cell Lung Cancer Under Therapy
Core Concepts
The author explores the genomic evolution of small cell lung cancer under therapy, highlighting key processes and patterns associated with sensitivity and resistance to chemotherapy.
Abstract
The study delves into the evolutionary processes of small cell lung cancer (SCLC) during treatment, revealing how chemotherapy impacts tumor heterogeneity. It identifies the common ancestor as a source of clonal diversity at relapse and uncovers genomic patterns linked to treatment response.
Treatment-naive SCLC tumors show clonal homogeneity, but chemotherapy induces intratumor heterogeneity and spatial diversity. Radio- or immunotherapy leads to re-expansion of founder clones with acquired genomic damage from previous treatments. Mutations in key genes like TP53 and RB1 are present in the common ancestor, while emerging subclonal mutations impact SCLC biology at relapse. Alterations in genes like CREBBP/EP300 are associated with genome duplications in tumors. Specific gene alterations are linked to shorter disease relapse post-chemotherapy, shedding light on sensitivity and resistance mechanisms.
Evolutionary trajectories of small cell lung cancer under therapy - Nature
Stats
MYC family amplifications were frequently not part of the founder clone.
Gene-damaging TP53 alterations were significantly associated with shorter disease relapse following chemotherapy.
Co-alterations of TP53 missense mutations with TP73, CREBBP/EP300 or FMN2 were linked to shorter disease relapse post-chemotherapy.
Quotes
Key Insights Distilled From
by Julie George... at www.nature.com 03-13-2024
https://www.nature.com/articles/s41586-024-07177-7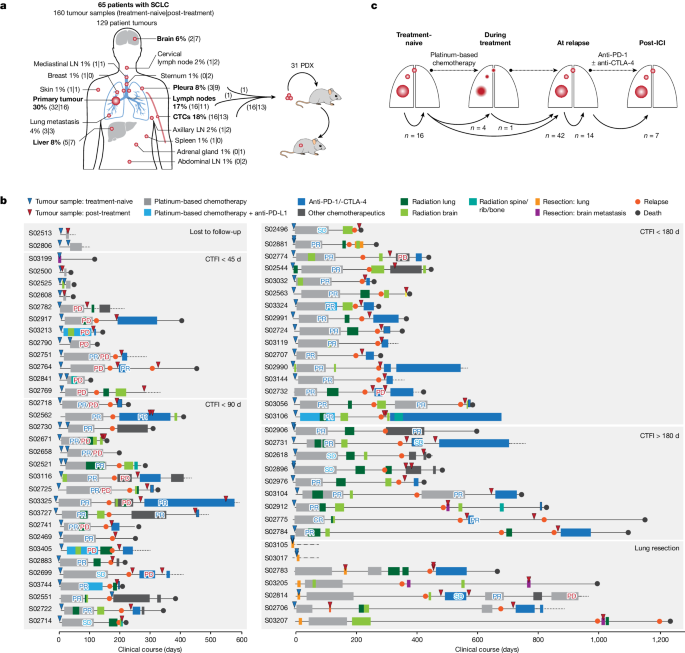
Deeper Inquiries
What implications does the identification of key genomic patterns have for personalized treatment approaches in SCLC
The identification of key genomic patterns in small cell lung cancer (SCLC) has significant implications for personalized treatment approaches. By understanding the evolutionary trajectories and genetic alterations that drive tumor progression, clinicians can tailor therapies to target specific vulnerabilities within the tumor. For example, identifying gene-damaging TP53 alterations or co-alterations with other genes associated with SCLC biology can help predict response to chemotherapy and guide treatment decisions. Personalized medicine strategies based on these genomic patterns can lead to more effective and targeted therapies, ultimately improving patient outcomes.
How might the presence of specific gene alterations impact future targeted therapies for small cell lung cancer
Specific gene alterations play a crucial role in shaping future targeted therapies for small cell lung cancer. The presence of mutations in genes such as TP53, RB1, MYC family members, CREBBP/EP300, and others can influence the response of tumors to different treatments. Targeted therapies designed to exploit these genetic vulnerabilities have the potential to enhance treatment efficacy while minimizing side effects. For instance, drugs targeting pathways affected by these gene alterations could be developed to specifically inhibit tumor growth or induce apoptosis in SCLC cells harboring those mutations. Understanding how these gene alterations impact tumor behavior is essential for developing precision medicine approaches that improve patient outcomes.
How can understanding the evolutionary trajectories of tumors under therapy improve overall patient outcomes
Understanding the evolutionary trajectories of tumors under therapy is crucial for improving overall patient outcomes in small cell lung cancer (SCLC). By tracking changes in intratumour heterogeneity and clonal diversity throughout treatment regimens, clinicians can adapt therapeutic strategies accordingly. For example, recognizing shifts towards ancestral clones at relapse or observing emerging subclonal mutations associated with resistance allows for timely adjustments in treatment plans. This knowledge enables healthcare providers to anticipate potential mechanisms of resistance and proactively address them through combination therapies or alternative treatment options. Ultimately, a deeper understanding of how tumors evolve under therapy empowers clinicians to make more informed decisions that maximize therapeutic benefits and prolong patient survival rates.
0
