Location Impact on Secondary Prevention After ICH
Core Concepts
Hematoma location in intracerebral hemorrhage (ICH) patients impacts the risk of major adverse cardiovascular events, guiding tailored prevention strategies.
Abstract
The study explores the impact of hematoma location in patients with intracerebral hemorrhage (ICH) on the risk of major adverse cardiovascular events (MACEs) and recurrent ICH. It aims to guide tailored secondary prevention approaches based on the location of the hemorrhage.
Highlights:
Patients with lobar ICH have a higher risk of MACEs compared to non-lobar ICH.
Recurrent ICH rates are significantly higher in lobar ICH patients.
Non-lobar ICH patients show increased risk of ischemic stroke and MI.
The study emphasizes the importance of optimal blood pressure control and other modifiable risk factors.
Hematoma location may help in risk stratification for secondary stroke prevention efforts.
ICH Location May Guide Secondary Prevention Strategy
Stats
"Results showed that after adjusting for potential confounders, compared with patients with non-lobar ICH, those with lobar ICH had higher rates of MACEs, with a rate per 100 person-years of 10.84 vs 7.91 (adjusted hazard ratio [aHR], 1.26)."
"This was driven by an increased rate of recurrent ICH (3.74 vs 1.24 per 100 person-years; aHR, 2.63)."
"However, rates of ischemic stroke and MI were numerically but not significantly higher in the non-lobar ICH group, with ischemic stroke rates per 100 person-years of 1.45 in those with lobar ICH vs 1.77 in those with non-lobar ICH (aHR, 0.81) and MI rates of 0.42 vs 0.64 (aHR, 0.64)."
Quotes
"This study helps us to identify the highest-risk patients with regard to tailoring secondary prevention approaches." - David Gaist, PhD
"Together, these findings may have potential clinical implications because they identify a group of vulnerable patients who might benefit from more targeted prevention efforts." - Study Authors
Key Insights Distilled From
by Sue Hughes at www.medscape.com 04-10-2023
https://www.medscape.com/viewarticle/990609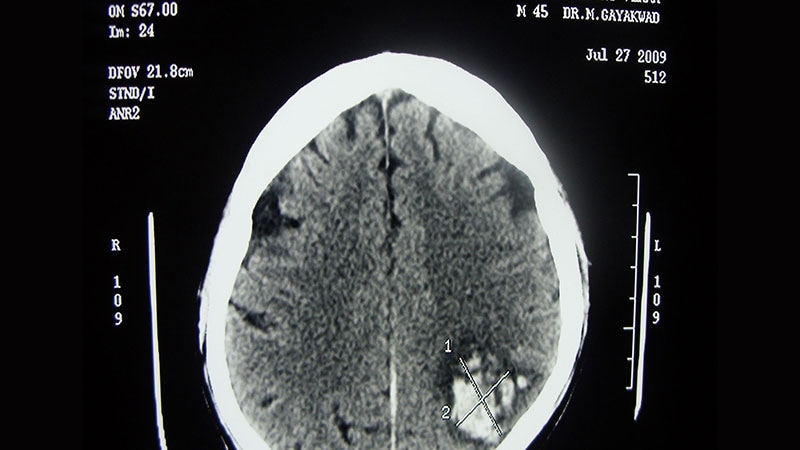
Deeper Inquiries
How can the findings of this study be practically implemented in clinical settings to improve patient outcomes?
The findings of this study can be practically implemented in clinical settings to improve patient outcomes by tailoring secondary prevention approaches based on the location of the intracerebral hemorrhage (ICH). For patients with lobar ICH, who have a higher risk of recurrent ICH, more focused monitoring and interventions to prevent another hemorrhagic event could be prioritized. This may involve close blood pressure control, lifestyle modifications, and potentially avoiding certain medications that could increase the risk of bleeding. On the other hand, for patients with non-lobar ICH, who are at increased risk of ischemic stroke and myocardial infarction, strategies such as early initiation of antithrombotic therapy, statins, and lifestyle modifications to address cardiovascular risk factors could be emphasized. By tailoring secondary prevention strategies based on hematoma location, healthcare providers can better address the specific risks faced by each group of patients, ultimately leading to improved outcomes.
What are the potential challenges in tailoring secondary prevention approaches based on hematoma location?
One potential challenge in tailoring secondary prevention approaches based on hematoma location is the need for accurate and timely identification of the location of the ICH. This may require advanced imaging techniques and expertise, which may not be readily available in all healthcare settings. Additionally, there could be variability in the interpretation of imaging results, leading to inconsistencies in treatment decisions. Another challenge is the complexity of managing multiple risk factors in patients with ICH, especially when they have comorbid conditions that may influence treatment choices. Balancing the need for preventing recurrent hemorrhagic events in lobar ICH patients while also addressing the increased risk of ischemic events in non-lobar ICH patients can be a delicate task. Furthermore, ensuring patient adherence to individualized prevention strategies and monitoring their response to treatment over time can pose additional challenges in clinical practice.
How might the study's emphasis on early risk identification impact current practices in cardiovascular event prevention?
The study's emphasis on early risk identification could significantly impact current practices in cardiovascular event prevention by highlighting the importance of timely intervention and close monitoring in patients with ICH. By identifying high-risk patients early based on hematoma location, healthcare providers can implement targeted prevention strategies soon after the initial event, potentially reducing the risk of recurrent cardiovascular events. This emphasis on early risk identification may lead to a shift towards more proactive and personalized approaches to cardiovascular event prevention, rather than waiting for complications to arise. Healthcare providers may start interventions such as blood pressure control, lifestyle modifications, and appropriate medication therapy sooner in the post-ICH period, aiming to mitigate the specific risks associated with each patient's hematoma location. Overall, the study's focus on early risk identification could lead to improved outcomes and a more tailored approach to cardiovascular event prevention in clinical practice.
0
