The Role of CGRP Sensory Neurons in Tissue Healing
Core Concepts
Nociceptive sensory neurons, specifically those expressing CGRP, play a crucial role in promoting tissue healing by modulating immune responses and enhancing repair processes.
Abstract
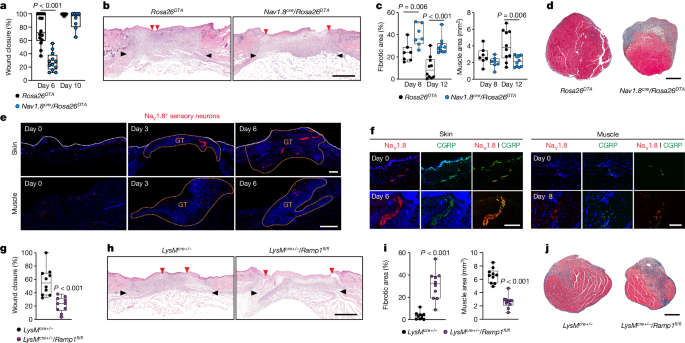
The immune system plays a vital role in tissue healing, especially in conditions like diabetes or advanced age that can impair the healing process. Nociceptive sensory neurons, particularly those expressing CGRP, have been found to influence tissue repair and regeneration following acute injury. Ablation of NaV1.8 nociceptors impairs skin wound repair and muscle regeneration. Nociceptor endings signal to immune cells through CGRP, affecting neutrophils, monocytes, and macrophages to promote tissue repair. CGRP acts via RAMP1 to inhibit recruitment, accelerate death, enhance efferocytosis, and polarize macrophages towards a pro-repair phenotype. The effects of CGRP are mediated via thrombospondin-1 release. In mice without nociceptors and diabetic mice, engineered CGRP accelerated wound healing and muscle regeneration, showing the potential of neuro-immune interactions in treating non-healing tissues.
Translate Source
To Another Language
Generate MindMap
from source content
Visit Source
www.nature.com
CGRP sensory neurons promote tissue healing via neutrophils and macrophages - Nature
Stats
Regenerative strategies controlling immune components have proven effective.
Nociceptive sensory neurons play a crucial role as immunoregulators.
Ablation of NaV1.8 nociceptors impairs skin wound repair and muscle regeneration.
CGRP acts via RAMP1 on neutrophils, monocytes, and macrophages to promote tissue repair.
Engineered CGRP accelerates wound healing and muscle regeneration in mice without nociceptors and diabetic mice.
Quotes
"Nociceptive sensory neurons have a crucial role as immunoregulators and exert both protective and harmful effects depending on the context."
"CGRP acts via receptor activity-modifying protein 1 (RAMP1) on neutrophils, monocytes, and macrophages to inhibit recruitment, accelerate death, enhance efferocytosis, and polarize macrophages towards a pro-repair phenotype."
Deeper Inquiries
How can the findings regarding CGRP and neuro-immune interactions be applied to other medical conditions beyond tissue healing
The findings regarding CGRP and neuro-immune interactions in tissue healing have significant implications for other medical conditions beyond just wound repair and muscle regeneration. By understanding how nociceptor endings signal to immune cells through CGRP to modulate immune responses, researchers can explore applications in conditions where immune dysregulation plays a role, such as autoimmune diseases, chronic inflammatory conditions, and even cancer. For instance, targeting CGRP-mediated pathways could potentially help in regulating immune responses in autoimmune disorders like rheumatoid arthritis or multiple sclerosis. Additionally, the ability of CGRP to influence macrophage polarization towards a pro-repair phenotype could be leveraged in enhancing tissue regeneration in various organ systems, not just skin and muscle. Overall, the insights gained from studying neuro-immune interactions in tissue healing open up avenues for developing novel therapeutic approaches in a wide range of medical conditions.
What potential challenges or limitations might arise in harnessing neuro-immune interactions for therapeutic purposes
While harnessing neuro-immune interactions for therapeutic purposes holds great promise, there are potential challenges and limitations that need to be considered. One challenge is the complexity of the neuro-immune crosstalk, as the interactions between the nervous system and immune system are intricate and multifaceted. Understanding the precise mechanisms and downstream effects of these interactions in different disease contexts can be challenging. Additionally, targeting specific neuro-immune pathways for therapeutic intervention may have unintended consequences, as these pathways often have pleiotropic effects and can impact multiple physiological processes simultaneously. Moreover, individual variability in neuro-immune responses could pose a challenge in developing universal therapeutic strategies that are effective across diverse patient populations. Furthermore, the potential for off-target effects or immune-related adverse reactions to neuro-modulatory therapies needs to be carefully evaluated to ensure safety and efficacy in clinical applications.
How can the understanding of neuro-immune interactions in tissue healing inspire research in other fields such as neurology or immunology
The understanding of neuro-immune interactions in tissue healing can inspire research in other fields such as neurology and immunology by shedding light on the intricate ways in which the nervous system and immune system communicate and collaborate. In neurology, insights from studying how nociceptor endings signal to immune cells through CGRP could provide new perspectives on neuroinflammatory processes in conditions like neurodegenerative diseases or neuropathic pain. Understanding how neuro-immune interactions influence tissue repair and regeneration could also inform research on neuroimmune disorders such as multiple sclerosis. In immunology, the knowledge gained from studying the effects of CGRP on immune cells could lead to novel approaches in modulating immune responses in various diseases, including autoimmune conditions and cancer. By bridging the gap between neurology and immunology through the lens of tissue healing, researchers can uncover new therapeutic targets and strategies for addressing a wide range of medical conditions.