Antibiotic Alternatives for Nontuberculous Mycobacterium: Bacteriophages and Inhaled NO
The content discusses the emergence of antibiotic alternatives for nontuberculous mycobacteria (NTM) pulmonary disease, focusing on bacteriophage therapy and inhaled nitric oxide (NO). Both treatments have shown efficacy in controlling persistent NTM infections, particularly Mycobacterium abscessus. Bacteriophages are viruses that target specific bacteria, while inhaled NO improves host defenses against infection. Clinical studies have demonstrated positive outcomes, with potential for these treatments to become adjunctive tools in managing challenging NTM infections.
- Bacteriophage Therapy:
- Highly targeted bactericidal effects
- Specific to the bacteria they infect
- Promising results in controlling M abscessus infections
- Inhaled Nitric Oxide (NO):
- Improves host defenses against infection
- Promising outcomes in controlling NTM infections
- Narrow therapeutic window poses challenges
The obstacles to widespread clinical application of these treatments are discussed, highlighting the need for further research to address limitations and define optimal regimens.
Customize Summary
Rewrite with AI
Generate Citations
Translate Source
To Another Language
Generate MindMap
from source content
Visit Source
www.medscape.com
Antibiotic Alternatives for Nontuberculous Mycobacterium
Key Insights Distilled From
by Ted Bosworth at www.medscape.com 07-27-2023
https://www.medscape.com/viewarticle/994878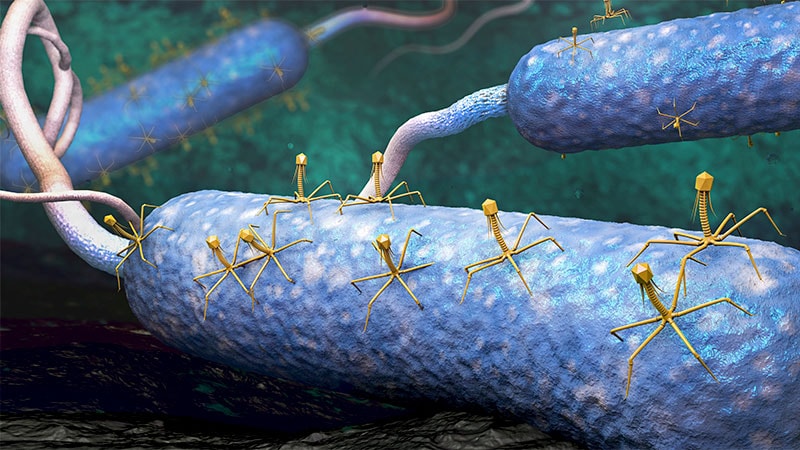
Deeper Inquiries
