Assessing Extended Criteria Hearts with OCS Heart Platform
Core Concepts
Using the OCS Heart platform for donor heart assessment significantly increases successful heart transplants, improving patient outcomes.
Abstract
TOPLINE:
- OCS Heart platform optimizes donor hearts.
- 87% of ECD hearts successfully transplanted.
- Potential to increase life-saving transplants.
METHODOLOGY:
- ECD hearts perfused using OCS Heart.
- ECD hearts defined by specific criteria.
- Primary outcome: patient survival and freedom from severe PGD.
- Secondary outcomes: donor heart use rate, survival, PGD incidence.
- Safety outcome: heart graft-related adverse events.
- 86.7% donor heart utilization rate.
TAKEAWAY:
- Reduced ischemic injury in donor hearts.
- Low incidence of severe LV or RV PGD.
- High patient survival and freedom from severe PGD.
- Low rate of serious adverse events.
IN PRACTICE:
- OCS Heart expands donor pool.
- Addresses limitations of cold storage.
- Increases heart transplants and patient access.
SOURCE:
- Study by Jacob N. Schroder, MD, Duke University Hospital.
- Published in JACC: Heart Failure on January 24, 2024.
LIMITATIONS:
- Single-arm design.
- Lack of risk-adjusted comparator.
- Use of lactate levels for heart suitability assessment.
DISCLOSURES:
- Study funded by TransMedics Inc.
- Research funding received by Schroder.
Customize Summary
Rewrite with AI
Generate Citations
Translate Source
To Another Language
Generate MindMap
from source content
Visit Source
www.medscape.com
Promising Method to Assess Extended Criteria Hearts
Stats
"87% of extended criteria donor (ECD) hearts being successfully transplanted"
"Donor heart utilization rate of 86.7%"
"Incidence of ISHLT severe LV or RV PGD was 6.7%"
"Overall survival for transplanted participants was 92.6% at 6 months"
Quotes
"Expanding the donor pool with OCS Heart could substantially increase the number of heart transplants and expand access to patients in need." - Authors
Key Insights Distilled From
by Pauline Ande... at www.medscape.com 01-30-2024
https://www.medscape.com/viewarticle/promising-method-assess-extended-criteria-hearts-2024a100021g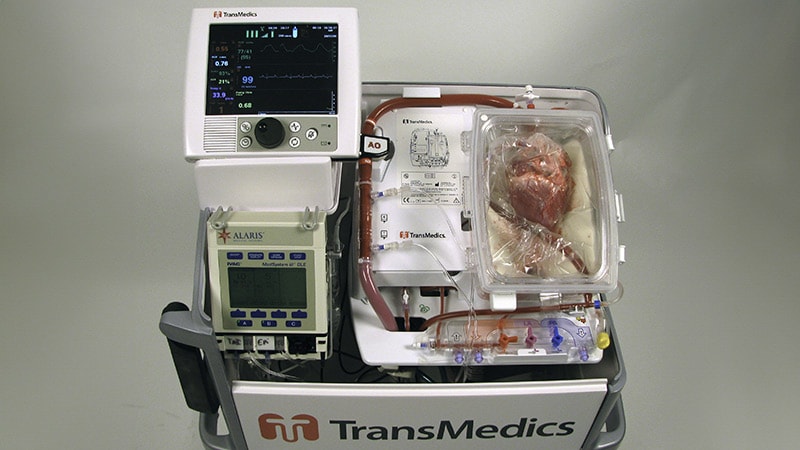
Deeper Inquiries
How can the use of OCS Heart impact the future of heart transplantation?
The utilization of the Organ Care System (OCS) Heart platform has the potential to revolutionize the field of heart transplantation by significantly increasing the number of viable donor hearts available for transplant. The OCS Heart platform allows for the perfusion, optimization, and assessment of extended criteria donor (ECD) hearts, which traditionally may have been deemed unsuitable for transplantation. By successfully transplanting 87% of ECD hearts in the trial, the OCS Heart platform demonstrates its ability to expand the donor pool and improve patient outcomes. This technology could address the limitations of cold storage for donor hearts and enable the safe utilization of ECD hearts, ultimately increasing access to life-saving heart transplants for patients in need.
What are the potential drawbacks of relying on the OCS Heart platform for heart assessments?
While the OCS Heart platform shows promising results in the assessment and transplantation of donor hearts, there are potential drawbacks to consider. One limitation is the single-arm design of the study, which may introduce bias and make it challenging to compare outcomes with a control group. Additionally, the reliance on OCS Heart circulating absolute lactate levels and perfusion parameters as biomarkers for heart suitability may not capture all relevant factors influencing transplant success. Further research is needed to determine if these biomarkers are the most effective indicators for clinical decision-making. Moreover, the financial implications of implementing OCS Heart technology on a larger scale, including costs associated with equipment, training, and maintenance, could pose challenges for widespread adoption.
How can advancements in heart transplant technology benefit other organ transplant procedures?
Advancements in heart transplant technology, such as the OCS Heart platform, have the potential to benefit other organ transplant procedures by improving organ assessment, preservation, and transplantation outcomes. Technologies developed for heart transplants, like the OCS Heart platform, could be adapted for use in other organ transplants, enhancing the viability of donor organs and expanding the donor pool. For example, innovations in organ perfusion and optimization could be applied to liver, lung, or kidney transplants, increasing the number of successful transplantations and improving patient survival rates. By sharing knowledge and techniques across different organ transplant fields, advancements in heart transplant technology can pave the way for enhanced practices and outcomes in other organ transplant procedures.
0
