Risk Factors for Different Rheumatoid Arthritis-Associated Interstitial Lung Disease Subtypes Identified
The study examined the risk factors associated with different subtypes of rheumatoid arthritis-associated interstitial lung disease (RA-ILD) using data from two cohorts in the Mass General Brigham Healthcare system.
The researchers identified 208 patients with RA-ILD and 547 control participants with rheumatoid arthritis (RA) but no ILD. RA-ILD subtypes were determined using high-resolution computed tomography (HRCT) imaging.
The key findings are:
- The RA-UIP subtype, which has the worst prognosis, was associated with older age at RA diagnosis, male sex, and seropositivity.
- The RA-NSIP subtype was significantly associated only with seropositivity.
- Nonfibrotic ILDs were significantly associated with positive smoking status and seropositivity.
- The combination of male sex, seropositivity, and positive smoking status was associated with a nearly sevenfold increased risk for RA-UIP.
The authors suggest that RA-ILD subtypes may have distinct risk factor profiles, emphasizing the importance of understanding RA-ILD disease heterogeneity to inform screening and prognostication strategies.
Customize Summary
Rewrite with AI
Generate Citations
Translate Source
To Another Language
Generate MindMap
from source content
Visit Source
www.medscape.com
RA Lung Disease Subtypes Have Distinct Risk Factor Profiles
Key Insights Distilled From
by Edited Javed... at www.medscape.com 09-26-2024
https://www.medscape.com/viewarticle/rheumatoid-arthritis-lung-disease-subtypes-have-distinct-2024a1000hhy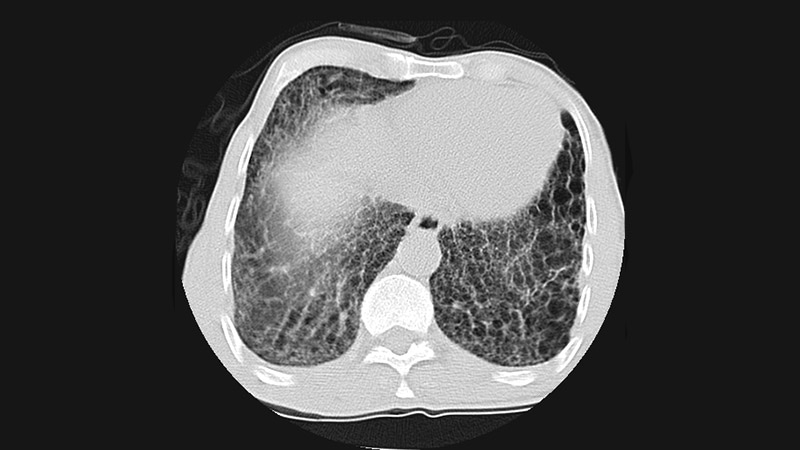
Deeper Inquiries
