Brain Frailty's Impact on Stroke Outcomes Across Ages
Core Concepts
Brain frailty significantly influences stroke outcomes across different ages.
Abstract
The content discusses how neuroimaging markers of brain frailty, such as brain atrophy, white matter disease, lacunes, and chronic infarctions, play a crucial role in mediating the association between age and functional outcomes after stroke. Here are the key highlights and insights:
Brain frailty markers mediate the link between age and post-stroke outcomes.
The burden of brain changes visible on neuroimaging is a significant factor in predicting stroke outcomes.
Neuroimaging features should be considered in clinical decision-making and future stroke trials.
Managing cardiovascular risk factors can potentially modify or prevent aspects of brain frailty.
The study emphasizes the importance of not solely relying on chronological age for outcome predictions and treatment decisions in stroke patients. Instead, incorporating neuroimaging features can provide a more nuanced prognostication and potentially improve patient care and research outcomes.
Brain Frailty Mediates Link Between Age and Stroke Outcomes
Stats
Markers of brain frailty mediate 85.1% of the total association of age with 90-day functional outcomes.
For every 10-year increase in age, there was a 0.47 percentage point increase in the mean modified Rankin Scale (mRS).
Composite frailty mediated nearly 100% of the total effect of age on functional outcomes.
For every 10-year increase in age, there was a 0.7 percentage point increase in the mean mRS.
Quotes
"To me, what is most interesting about our study is that it implies that most of the association of chronological age with worse outcomes after stroke relates to the burden of brain changes that we can readily observe on routinely acquired neuroimaging." - Aravind Ganesh, MD
"While chronological age is one of the most influential determinants of poststroke outcomes, little is known of the impact of neuroimaging-derived biological brain age." - Oscar Benavente, MD
Key Insights Distilled From
by Carolyn Cris... at www.medscape.com 01-15-2024
https://www.medscape.com/viewarticle/brain-frailty-mediates-link-between-age-and-stroke-outcomes-2024a10000w6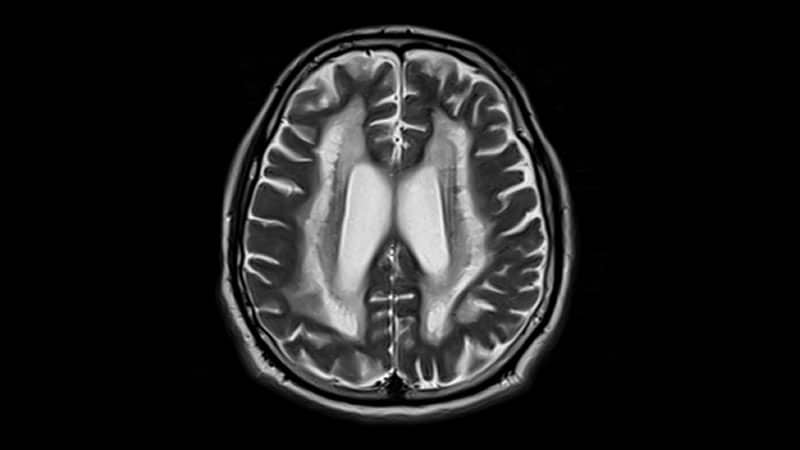
Deeper Inquiries
How can the concept of brain frailty be applied to other neurological conditions beyond stroke
The concept of brain frailty, as highlighted in the context of stroke outcomes, can be extended to other neurological conditions beyond stroke. For instance, in conditions like traumatic brain injury, intracerebral hemorrhage, and demyelinating disorders, similar neuroimaging markers of brain frailty could play a crucial role in predicting outcomes. In traumatic brain injury, the presence of brain atrophy, white matter disease, and chronic infarctions could indicate the extent of damage and potential recovery trajectory. In demyelinating disorders like multiple sclerosis, neuroimaging markers could help assess disease progression and response to treatment. By identifying and quantifying these markers, healthcare providers can tailor interventions and prognostic discussions to individual patients, leading to more personalized and effective care strategies.
What are the potential limitations of solely relying on neuroimaging markers for outcome predictions in stroke patients
While neuroimaging markers of brain frailty offer valuable insights into predicting outcomes in stroke patients, there are potential limitations to solely relying on these markers for outcome predictions. One limitation is the static nature of neuroimaging data, which may not capture dynamic changes in the brain over time. Patients' responses to treatment, rehabilitation, or other interventions may not be fully reflected in baseline neuroimaging assessments. Additionally, neuroimaging markers may not account for individual variations in resilience, cognitive reserve, or other factors that could influence recovery. Therefore, integrating clinical assessments, functional evaluations, and patient-reported outcomes alongside neuroimaging data is essential for a comprehensive understanding of stroke outcomes. A multidimensional approach that combines various assessments can provide a more holistic view of a patient's prognosis and guide personalized treatment plans.
How might the integration of neuroimaging features in stroke care impact healthcare disparities among different patient populations
The integration of neuroimaging features in stroke care has the potential to impact healthcare disparities among different patient populations in several ways. Firstly, by incorporating neuroimaging markers of brain frailty into prognostic models, healthcare providers can offer more accurate and tailored predictions of outcomes for diverse patient groups. This personalized approach can help address disparities in access to specialized care, rehabilitation services, and resources based on individual risk profiles. Secondly, by considering neuroimaging data alongside clinical and demographic factors, healthcare teams can identify high-risk patients from underserved communities who may benefit from targeted interventions or closer monitoring. This proactive approach can help mitigate disparities in stroke care outcomes by ensuring that all patients receive appropriate and timely interventions based on their unique neuroimaging profiles. Ultimately, the integration of neuroimaging features in stroke care can contribute to more equitable healthcare delivery and improved outcomes for patients across different populations.
0
