Isoniazid Resistance Linked to Higher Tuberculosis Death Rates in Brazil
Core Concepts
Isoniazid monoresistance is associated with higher rates of unfavorable tuberculosis treatment outcomes, including death, in Brazil, highlighting the need for improved drug sensitivity testing.
Abstract
The content discusses the issue of isoniazid resistance in tuberculosis (TB) treatment in Brazil. Key points:
- In 2022, Brazil reported over 78,000 new TB cases, with an incidence of 36.3 cases per 100,000 inhabitants.
- Researchers from the Regional Prospective Observational Research for Tuberculosis (RePORT)-Brazil consortium found that monoresistance to isoniazid, a key first-line TB drug, predicted unfavorable treatment outcomes at the national level.
- While Brazil's Ministry of Health recommends sensitivity testing for all suspected TB cases since 2015, in practice, only about 30% of cases undergo culture testing, and only 12% have sensitivity testing to identify resistance to first- and second-line drugs.
- The study analyzed 21,197 TB cases and found a 1.4% rate of isoniazid monoresistance.
- Patients with isoniazid monoresistance had significantly higher rates of unfavorable outcomes, such as death or treatment failure (9.1% vs. 3.05%), compared to those without resistance.
- Researchers emphasize the importance of implementing comprehensive drug sensitivity testing before starting TB treatment to enable more targeted and effective therapies, which can help prevent the transmission of resistant strains and improve treatment outcomes.
- Implementing this testing in Brazil's public health system requires improvements in resource allocation, coordination between national and local TB programs, and upgrades to infrastructure and technical capacity of public health laboratories.
Customize Summary
Rewrite with AI
Generate Citations
Translate Source
To Another Language
Generate MindMap
from source content
Visit Source
www.medscape.com
Isoniazid Resistance Linked With Tuberculosis Deaths
Stats
In 2022, Brazil reported over 78,000 new TB cases, with an incidence of 36.3 cases per 100,000 inhabitants.
The study analyzed 21,197 TB cases registered in Brazil between June 2015 and June 2019 and found a 1.4% rate of isoniazid monoresistance.
The frequency of unfavorable outcomes (death or treatment failure) was significantly higher among patients with isoniazid monoresistance (9.1% vs. 3.05%).
Quotes
"This not only increases the chances of successful individual treatment but also helps prevent the transmission of resistant strains and develop a more accurate understanding of drug resistance trends."
"Although the initial cost is considerable, these investments can be offset by long-term savings resulting from the reduction in the use of more expensive and prolonged treatments for resistant tuberculosis."
Key Insights Distilled From
by Teresa Santo... at www.medscape.com 03-28-2024
https://www.medscape.com/viewarticle/isoniazid-resistance-linked-tuberculosis-deaths-2024a10005vw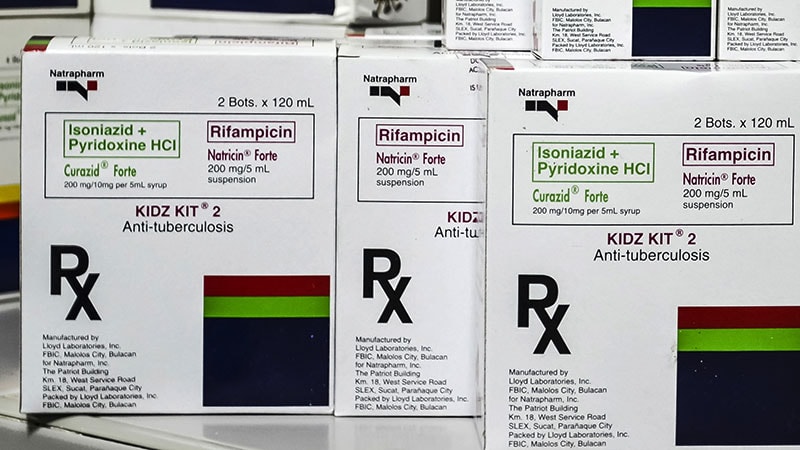
Deeper Inquiries
What are the potential barriers to implementing comprehensive drug sensitivity testing for TB patients in Brazil's public health system, and how can they be overcome?
In Brazil, potential barriers to implementing comprehensive drug sensitivity testing for TB patients in the public health system include limited resources, inadequate infrastructure, and a lack of coordination between national, state, and municipal programs. The high cost associated with sensitivity testing, the shortage of technical staff trained to conduct these tests, and the current low rates of testing in practice are significant challenges. To overcome these barriers, it is crucial to improve resource allocation, enhance coordination between different levels of the health system, invest in infrastructure and training for technical staff, and increase the availability of testing facilities. Strengthening partnerships between the national TB program and local health authorities can help streamline the testing process and ensure that all TB patients have access to comprehensive sensitivity testing before starting treatment.
How do the treatment outcomes and transmission dynamics of isoniazid-resistant TB compare to other forms of drug-resistant TB in Brazil?
The study highlighted in the context indicates that monoresistance to isoniazid in TB patients is associated with unfavorable treatment outcomes, including a higher frequency of death or therapeutic failure compared to patients without isoniazid resistance. Specifically, patients with isoniazid resistance had a significantly higher rate of unfavorable outcomes (9.1% vs. 3.05%). This suggests that isoniazid-resistant TB poses a greater risk in terms of treatment success and patient survival. Furthermore, the transmission dynamics of isoniazid-resistant TB can contribute to the spread of resistant strains, potentially leading to more challenging control efforts. Compared to other forms of drug-resistant TB, isoniazid resistance may have a unique impact on treatment outcomes and transmission dynamics, underscoring the importance of early detection and targeted interventions.
What innovative approaches or technologies could be leveraged to improve access to drug sensitivity testing and optimize TB treatment in resource-limited settings like Brazil?
In resource-limited settings like Brazil, leveraging innovative approaches and technologies can help improve access to drug sensitivity testing and optimize TB treatment. One such approach is the use of point-of-care molecular diagnostic tests, such as the Xpert MTB/RIF Ultra assay, which can rapidly detect TB and rifampicin resistance in a single test. These tests are user-friendly, have a quick turnaround time, and can be deployed in decentralized settings, making them suitable for resource-limited environments. Additionally, telemedicine and digital health platforms can facilitate remote consultation and support for healthcare providers in interpreting test results and managing TB cases effectively. Mobile health applications can also be utilized to enhance patient monitoring and adherence to treatment regimens. By integrating these innovative approaches and technologies into the existing healthcare infrastructure, Brazil can enhance access to drug sensitivity testing, improve treatment outcomes, and ultimately strengthen TB control efforts.
0
