Atopic Dermatitis Linked to GBS Colonization in Pregnancy
Concetti Chiave
Atopic dermatitis increases GBS colonization risk in pregnant women.
Sintesi
The study suggests that pregnant women with atopic dermatitis (AD) are more likely to be colonized with group B streptococcus (GBS) compared to others. Researchers conducted a cross-sectional study using an administrative database to explore this association. Key findings include:
AD may be a risk factor for maternal carriage of GBS.
Women with AD had higher odds of asthma and seasonal allergies.
GBS was reported in 20.6% of the cohort.
Pregnant women with AD had a higher prevalence of GBS colonization.
Individuals with AD might have deficiencies in host defenses against pathogens.
Antibiotic use in AD treatment could alter the resident microbiome.
The study acknowledges limitations due to the reliance on an administrative database.
Adam Friedman highlighted the importance of screening pregnant AD patients for GBS and raised questions about potential changes in clinical practices. The study does not provide definitive answers but prompts further inquiry into screening and decolonization regimens for pregnant women with AD.
AD May Be a Risk Factor for GBS Colonization in Pregnancy
Statistiche
"GBS was reported in 20.6% of the cohort."
"Among the women with AD, 24.1% had GBS, compared with 20.51% of the women without AD (P <.0001)."
"The OR of asthma was 1.08 (95% CI, 1.06-1.10) among women with GBS."
Citazioni
"AD could be a risk factor for maternal carriage of GBS."
"Individuals with AD frequently receive antibiotics as part of their AD treatment and this might alter their resident microbiome."
"Pregnant women should be screened for GBS regardless, but maybe more attention or counseling can be offered to AD patients about the importance of screening."
Approfondimenti chiave tratti da
by Doug Brunk alle www.medscape.com 08-25-2023
https://www.medscape.com/viewarticle/995867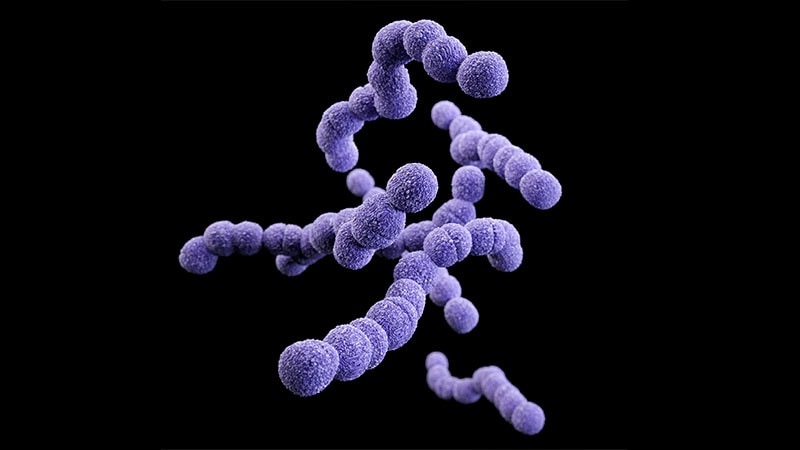
Domande più approfondite
What are the implications of GBS colonization in pregnant women with atopic dermatitis beyond pregnancy outcomes?
Pregnant women with atopic dermatitis (AD) who are colonized with group B streptococcus (GBS) may face implications beyond pregnancy outcomes. GBS colonization in pregnant women with AD could potentially lead to an increased risk of vertical transmission of GBS to the newborn during delivery, which can result in neonatal GBS infection. Neonatal GBS infection can manifest as early-onset disease, presenting within the first week of life, or late-onset disease, occurring between the first week and several months of life. Both forms of GBS infection can have serious consequences, including sepsis, pneumonia, and meningitis, which can be life-threatening for the newborn. Therefore, the implications of GBS colonization in pregnant women with AD extend to the health and well-being of the newborn, highlighting the importance of addressing GBS colonization in this population.
How might the findings of this study impact the management of atopic dermatitis in pregnant women?
The findings of the study suggesting an association between atopic dermatitis (AD) and group B streptococcus (GBS) colonization in pregnant women have significant implications for the management of AD in this population. Healthcare providers caring for pregnant women with AD should be aware of the increased likelihood of GBS colonization in these patients. This awareness can prompt healthcare providers to consider GBS screening and appropriate management strategies for pregnant women with AD to reduce the risk of GBS colonization and potential vertical transmission to the newborn. Additionally, the study findings underscore the importance of a multidisciplinary approach to the management of AD in pregnant women, involving dermatologists, obstetricians, and infectious disease specialists to optimize care and outcomes for both the mother and the newborn.
How can the dysbiosis associated with atopic dermatitis be effectively addressed to reduce the risk of GBS colonization?
Addressing the dysbiosis associated with atopic dermatitis (AD) to reduce the risk of group B streptococcus (GBS) colonization in pregnant women requires a comprehensive approach. Strategies to restore microbial balance and reduce dysbiosis in pregnant women with AD may include the use of emollients and moisturizers to support the skin barrier function, which can help prevent pathogen colonization. Additionally, promoting a healthy skin microbiome through the use of probiotics or prebiotics may help restore microbial diversity and inhibit the growth of pathogenic bacteria like GBS. Proper skincare routines, avoidance of triggers that exacerbate AD symptoms, and adherence to prescribed treatments can also play a crucial role in maintaining skin health and reducing dysbiosis. Collaborative efforts between dermatologists, obstetricians, and other healthcare providers can ensure a holistic approach to addressing dysbiosis in pregnant women with AD, ultimately reducing the risk of GBS colonization and its associated complications.
0
