ApoA1 Infusion Fails to Reduce Cardiovascular Events in Acute MI Patients, But May Benefit Those with High LDL Levels
Grunnleggende konsepter
An ApoA1 infusion product did not significantly reduce the primary composite endpoint of cardiovascular death, myocardial infarction, or stroke in patients with acute MI and additional risk factors. However, an exploratory analysis showed significant benefits in patients with higher baseline LDL levels.
Sammendrag
The AEGIS-II trial evaluated the efficacy of an ApoA1 infusion product, CSL112, in reducing cardiovascular events in 18,219 patients with acute myocardial infarction (MI) and additional risk factors.
Key Highlights:
The primary composite endpoint of cardiovascular death, MI, or stroke at 90 days was not significantly different between the CSL112 and placebo groups (4.8% vs 5.2%).
At 180 days and 1 year, the event rates were also not significantly different between the two groups.
However, the CSL112 group had a lower number of MI and cardiovascular death events but a higher number of strokes compared to placebo.
An exploratory analysis showed that in patients with baseline LDL levels above 100 mg/dL, CSL112 was associated with significant reductions in the primary composite endpoint at all timepoints (90 days, 180 days, and 1 year).
In contrast, there was no effect of CSL112 in patients with baseline LDL levels below 100 mg/dL.
The researchers suggest the results are biologically plausible, as patients with higher LDL levels are more likely to have lipid-rich atherosclerotic plaques that could benefit from the plaque-stabilizing effects of ApoA1.
The safety profile of CSL112 was similar to placebo, although there were more hypersensitivity events reported in the CSL112 group.
ApoA1 Trial Misses Endpoint, But HDL Hypothesis Still Alive?
Statistikk
The primary composite endpoint occurred in 4.8% of the CSL112 group versus 5.2% of the placebo group at 90 days (HR 0.93, 95% CI 0.81-1.05, p=0.24).
At 180 days, the endpoint occurred in 6.9% of the CSL112 group versus 7.6% of the placebo group (HR 0.91, 95% CI 0.81-1.01).
At 1 year, the event rate was 9.8% versus 10.5% (HR 0.93, 95% CI 0.85-1.02).
In patients with baseline LDL > 100 mg/dL, the primary endpoint occurred in 3.4% of the CSL112 group versus 4.9% of the placebo group at 90 days (HR 0.69, 95% CI 0.53-0.90, p=0.007).
Sitater
"If a patient doesn't have a lot of excess lipid in their plaques then a therapy to remove lipids from the plaques is not going to help."
"What I take from these results is that we need to be more aggressive in lowering LDL."
"Although there was no significant reduction in the incidence of the primary composite endpoint, a positive trend was seen with respect to the individual component of MI that could be consistent with the proposed biologic effect."
Viktige innsikter hentet fra
by klokken www.medscape.com 04-06-2024
https://www.medscape.com/viewarticle/apoa1-trial-misses-endpoint-hdl-hypothesis-still-alive-2024a10006km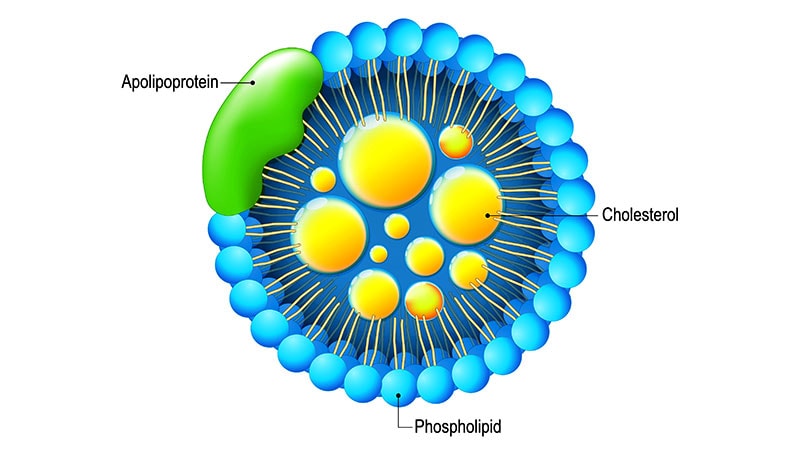
Dypere Spørsmål
How can the findings from the exploratory analysis be prospectively verified in a future clinical trial?
To prospectively verify the findings from the exploratory analysis in a future clinical trial, researchers can design a randomized controlled trial specifically focusing on patients with baseline LDL levels above 100 mg/dL. This trial should include a larger sample size to ensure statistical power and robust results. Patients should be randomized to receive either the ApoA1 infusion therapy or a placebo, and the primary composite endpoint should be assessed at multiple timepoints, similar to the exploratory analysis. By conducting a well-designed trial with predefined endpoints and statistical analysis plans, researchers can validate the observed benefits of ApoA1 therapy in patients with higher LDL levels.
What other patient characteristics, beyond just LDL levels, could help identify the subgroup most likely to benefit from ApoA1 infusion therapy?
In addition to LDL levels, other patient characteristics that could help identify the subgroup most likely to benefit from ApoA1 infusion therapy include:
High-risk Plaque Features: Patients with high-risk plaque characteristics, such as vulnerable plaques prone to rupture, may benefit more from ApoA1 therapy due to its plaque-stabilizing effects.
Inflammatory Markers: Patients with elevated inflammatory markers, such as high-sensitivity C-reactive protein (hs-CRP), may have a higher burden of inflammation in their plaques, making them potential candidates for ApoA1 therapy.
Genetic Factors: Genetic predispositions related to lipid metabolism and cholesterol efflux pathways could influence the response to ApoA1 therapy. Genetic testing may help identify patients who are more likely to benefit from this treatment.
Previous Cardiovascular Events: Patients with a history of recurrent cardiovascular events despite standard therapies may represent a subgroup that could benefit from ApoA1 infusion therapy to address underlying lipid-related mechanisms contributing to their disease.
By considering a combination of these patient characteristics in addition to LDL levels, clinicians and researchers can better tailor ApoA1 therapy to individuals who are most likely to derive clinical benefits.
Given the potential plaque-stabilizing effects of ApoA1, are there other cardiovascular conditions beyond acute MI where this therapy could be investigated?
Yes, there are several other cardiovascular conditions beyond acute MI where ApoA1 therapy could be investigated due to its potential plaque-stabilizing effects. Some of these conditions include:
Unstable Angina: Patients with unstable angina often have vulnerable plaques that are prone to rupture, leading to acute coronary events. ApoA1 therapy could potentially stabilize these plaques and reduce the risk of plaque rupture and subsequent events.
Carotid Artery Disease: Atherosclerotic plaques in the carotid arteries can lead to stroke if they rupture or cause significant stenosis. ApoA1 therapy may help stabilize these plaques and reduce the risk of cerebrovascular events.
Peripheral Artery Disease (PAD): Patients with PAD often have atherosclerotic plaques in their peripheral arteries, leading to reduced blood flow and increased risk of limb ischemia. ApoA1 therapy could potentially improve plaque stability in peripheral arteries and reduce the risk of adverse limb events.
Coronary Artery Disease (CAD): Beyond acute MI, patients with stable CAD or those who have undergone revascularization procedures may benefit from ApoA1 therapy to prevent future cardiovascular events by stabilizing atherosclerotic plaques in the coronary arteries.
By exploring the use of ApoA1 therapy in these cardiovascular conditions, researchers can further elucidate its potential benefits in stabilizing plaques and reducing the overall burden of atherosclerotic disease.
0
