High Biomarker Level Plus Diabetes Predict Bad PCI Outcomes
Grunnleggende konsepter
High platelet-to-lymphocyte ratio (PLR) in patients with type 2 diabetes undergoing PCI increases the risk of adverse cardiovascular events and stent thrombosis.
Sammendrag
The study focused on the impact of the platelet-to-lymphocyte ratio (PLR) on patients with type 2 diabetes undergoing percutaneous coronary intervention (PCI). Here are the key points:
Key Takeaways
High PLR in diabetic patients undergoing PCI linked to increased risk of MACCE and stent thrombosis.
PLR not associated with adverse outcomes in non-diabetic patients.
Why This Matters
PLR serves as an inflammatory biomarker.
Previous studies highlight PLR's significance in evaluating disease activity and prognosis in various disorders.
Study Design
8831 adults who underwent PCI were analyzed.
Patients with high PLR had higher risks of MACCE and stent thrombosis.
Patients with type 2 diabetes and high PLR require close monitoring post-PCI.
Key Results
High PLR in diabetic patients associated with increased risk of MACCE and stent thrombosis.
No significant risk increase in non-diabetic patients with high PLR.
Limitations
Observational study with potential unadjusted confounders.
Lack of data on PLR and glycemic status changes during follow-up.
Findings may have limited generalizability due to the exclusively Chinese population.
High Biomarker Level Plus Diabetes Predict Bad PCI Outcomes
Statistikk
Among patients with type 2 diabetes, those with a high PLR had a significantly higher risk of MACCE compared with those with a low PLR (hazard ratio, 1.53) and stent thrombosis (hazard ratio, 3.79).
During a median 2.4-year follow-up, 663 patients (7.5%) had MACCE and 75 patients (0.85%) had stent thrombosis.
Sitater
"PLR is an easy-to-obtain inflammatory biomarker."
"Results suggest that patients with type 2 diabetes and a high PLR should be closely monitored following PCI."
Viktige innsikter hentet fra
by Marlene Busk... klokken www.medscape.com 03-28-2023
https://www.medscape.com/viewarticle/990192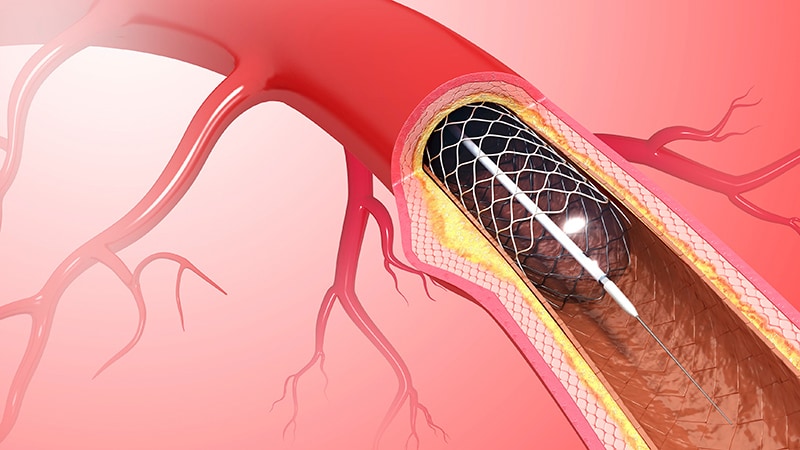
Dypere Spørsmål
How can the findings of this study impact the treatment strategies for diabetic patients undergoing PCI
The findings of this study can significantly impact the treatment strategies for diabetic patients undergoing PCI. By identifying a high platelet-to-lymphocyte ratio (PLR) as an independent risk factor for stent thrombosis and major adverse cardiovascular and cerebrovascular events (MACCE) in diabetic patients post-PCI, healthcare providers can now incorporate PLR measurements into their risk assessment protocols. This means that diabetic patients with a high PLR should be closely monitored following PCI to mitigate the increased risk of adverse outcomes. Additionally, healthcare professionals can tailor treatment plans for diabetic patients based on their PLR levels, potentially adjusting medications or interventions to improve patient outcomes and reduce the risk of complications post-PCI.
What potential biases could arise from the study's exclusive focus on a Chinese population
The exclusive focus on a Chinese population in this study may introduce potential biases that could limit the generalizability of the findings to other populations. One bias that could arise is population-specific genetic variations that may impact the relationship between PLR and outcomes post-PCI. Additionally, cultural or lifestyle factors unique to the Chinese population may influence the results and limit their applicability to more diverse populations. Furthermore, healthcare practices and access to medical care in China may differ from those in other countries, affecting the outcomes observed in this study. Therefore, it is essential to replicate this research in diverse populations to validate the findings and ensure that they can be applied globally.
How might the concept of using PLR as a biomarker extend to other medical conditions beyond cardiovascular diseases
The concept of using platelet-to-lymphocyte ratio (PLR) as a biomarker can extend beyond cardiovascular diseases to other medical conditions due to its role as an inflammatory marker. PLR has shown promise in assessing disease activity, treatment response, and prognosis in various inflammatory disorders such as solid tumors, arthritis, and acute kidney injury. Given its association with inflammation and poor prognosis in cardiovascular diseases like ST-elevation myocardial infarction and heart failure, PLR could potentially be utilized in monitoring and predicting outcomes in a wide range of medical conditions characterized by inflammation. By measuring PLR levels, healthcare providers may gain valuable insights into the inflammatory burden and prognosis of patients, allowing for more personalized and effective treatment strategies across different medical specialties.
0
