HPV Vaccination Impact on Cervical Lesion Progression
Główne pojęcia
HPV vaccination before age 20 reduces the risk of cervical lesion progression.
Streszczenie
TOPLINE:
- HPV vaccination before age 20 linked to lower progression odds in CIN2 women.
METHODOLOGY:
- Study on 7904 Danish women with CIN2 undergoing surveillance.
- CIN2 lesions may regress naturally, removal can increase preterm birth risk.
TAKEAWAY:
- Progression risk: 22.9% for <15, 31.5% for 15-20, 37.6% for unvaccinated.
- <15 vaccination group had 35% lower progression risk.
- Cervical cancer rates: 0.37% unvaccinated, 0.13% vaccinated.
- All cervical cancer cases in vaccinated group were after age 20 vaccination.
IN PRACTICE:
- HPV vaccination status can help identify high-risk women at CIN2 diagnosis.
SOURCE:
- Study by Louise Krog, BscMed, Aarhus University, published in AJOG.
LIMITATIONS:
- Limited data on smoking, immunosuppression, and sexual activity age.
DISCLOSURES:
- Study funded by Danish Cancer Society, Carpenter Axel Kastrup-Nielsen's Memorial Fund, and Dagmar Marshall's Fund. Coauthors have ties to AstraZeneca, Roche, and Hologic.
Dostosuj podsumowanie
Przepisz z AI
Generuj cytaty
Przetłumacz źródło
Na inny język
Generuj mapę myśli
z treści źródłowej
Odwiedź źródło
www.medscape.com
HPV Vax Tied to Lower Odds of Cervical Lesion Progression
Statystyki
Nearly half of the women had received at least one dose of an HPV vaccine at least 1 year before the diagnosis of cervical dysplasia.
Women vaccinated before age 15 had a 35% lower risk for progression than unvaccinated women, after adjusting for cytology, income, and education (adjusted relative risk, 0.65; 95% CI, 0.57-0.75).
Cervical cancer developed in 0.37% of the unvaccinated women and 0.13% of the vaccinated women.
Cytaty
"These findings suggest that HPV vaccination status may be used to identify women at higher risk for progression, thereby enabling risk stratification at the time of CIN2 diagnosis."
Kluczowe wnioski z
by Jake Remaly o www.medscape.com 01-11-2024
https://www.medscape.com/viewarticle/hpv-vax-tied-lower-odds-cervical-lesion-progression-2024a10000pm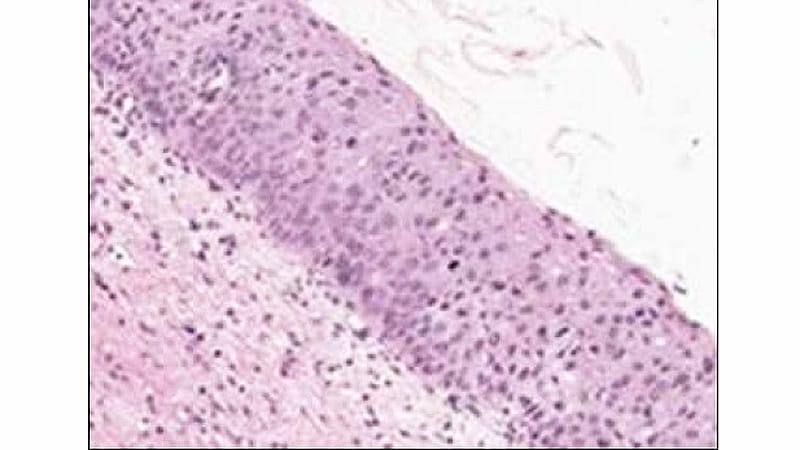
Głębsze pytania
How can the findings of this study impact public health policies regarding HPV vaccination?
The findings of this study can have significant implications for public health policies related to HPV vaccination. By demonstrating that HPV vaccination before the age of 20 is associated with lower odds of progression in women with CIN2, policymakers may consider expanding vaccination programs to target this specific demographic. Public health authorities could use this data to prioritize HPV vaccination for young women to reduce the risk of cervical lesion progression and potentially prevent cervical cancer. Additionally, the study suggests that HPV vaccination status could be used as a tool for risk stratification at the time of CIN2 diagnosis, which could inform personalized treatment plans and improve outcomes for patients.
What potential biases could arise due to the lack of information on smoking, immunosuppressive conditions, and sexual activity age?
The lack of information on smoking, immunosuppressive conditions, and age at which patients became sexually active in the study could introduce several biases. Smoking is a known risk factor for cervical cancer and could confound the relationship between HPV vaccination and lesion progression. Immunosuppressive conditions may impact the body's response to the vaccine and influence disease progression. Additionally, the age at which patients became sexually active is a crucial factor in HPV transmission and infection. Without considering these variables, the study results may be skewed or incomplete, leading to inaccurate conclusions about the effectiveness of HPV vaccination in preventing cervical lesion progression.
How can the study's focus on HPV vaccination in CIN2 women be extrapolated to other demographics or diseases?
While the study specifically focused on HPV vaccination in women with CIN2, the findings can be extrapolated to other demographics and diseases with similar risk factors. The concept of using vaccination status for risk stratification could be applied to different populations at risk of developing HPV-related diseases, such as men who have sex with men or individuals with compromised immune systems. Additionally, the study's emphasis on the timing of vaccination before age 20 could be relevant for other age groups or diseases where early intervention is crucial. By understanding the impact of HPV vaccination on disease progression in CIN2 women, researchers and policymakers can explore how these insights can be translated to diverse populations to improve preventive healthcare strategies.
0
