Anticoagulation in ESUS with Atrial Cardiopathy
The ARCADIA trial compared apixaban to aspirin in ESUS patients with atrial cardiopathy, finding no improvement in recurrent stroke rates or safety outcomes. The study presenter highlighted the lack of benefit of apixaban over aspirin in this patient population. Secondary analyses will be conducted to explore potential explanations. Similar results were seen in previous ESUS trials. The definition of atrial cardiopathy and the heterogeneity of patients were discussed. The failure of anticoagulation in previous trials led to the hypothesis of different underlying etiologies requiring varied antithrombotic therapy. The trial methodology, patient characteristics, outcomes, and safety results were detailed. Twitter reactions from experts were also included.
客製化摘要
使用 AI 重寫
產生引用格式
翻譯原文
翻譯成其他語言
產生心智圖
從原文內容
前往原文
www.medscape.com
Cardiopathy No Basis for Choosing Anticoagulation in ESUS
從以下內容提煉的關鍵洞見
by Liam Davenpo... 於 www.medscape.com 05-29-2023
https://www.medscape.com/viewarticle/992525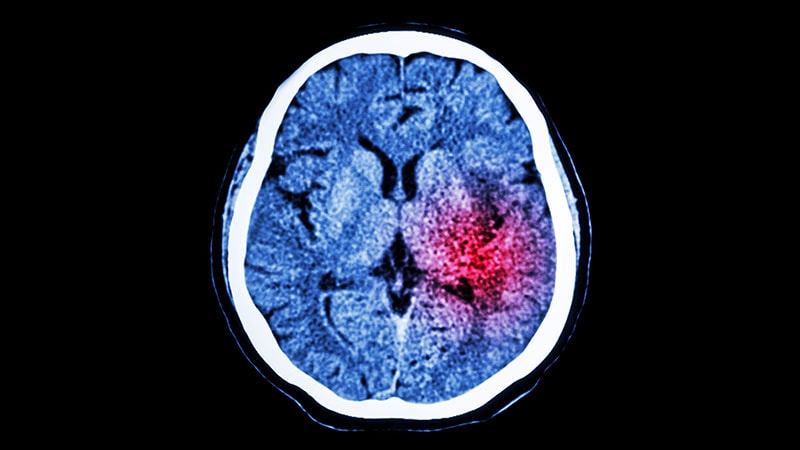
深入探究
