Accuracy of Preoperative EAC Biopsies in Predicting Tumor Grade
Основні поняття
Preoperative biopsies for esophageal adenocarcinoma often misrepresent true tumor grade, impacting treatment decisions.
Анотація
The study highlights the discrepancy between preoperative biopsy results and actual tumor grade in esophageal adenocarcinoma (EAC) patients. It questions the accuracy of endoscopic biopsies for clinical decision-making and emphasizes the potential risks of unnecessary esophagectomy due to inaccurate preoperative findings. The research compares biopsy results with both surgical and endoscopic resection specimens, revealing significant discrepancies in tumor differentiation. Notably, a considerable percentage of tumors were upgraded or downgraded upon final histology, impacting treatment choices and the need for more precise diagnostic methods.
Many Preop EAC Biopsies Fail to Predict True Tumor Grade
Статистика
Preoperative biopsy accuracy: 68%
Esophagectomy group accuracy: 72%
ER group accuracy: 56%
22.7% of moderately differentiated tumors were upgraded to poorly differentiated upon final histology.
19.6% of poorly differentiated tumors were downgraded to moderately differentiated.
40% of T1a tumors were changed from poorly to moderately differentiated between pre- and postprocedural histology.
Цитати
"Inaccurate preoperative biopsy findings could mean that patients who are candidates for endoscopic resection (ER) are unnecessarily undergoing esophagectomy."
"If poor differentiation was the only high-risk feature, these patients may have unnecessarily undergone esophagectomy."
Ключові висновки, отримані з
by Will Pass о www.medscape.com 11-09-2023
http://www.medscape.com/viewarticle/998305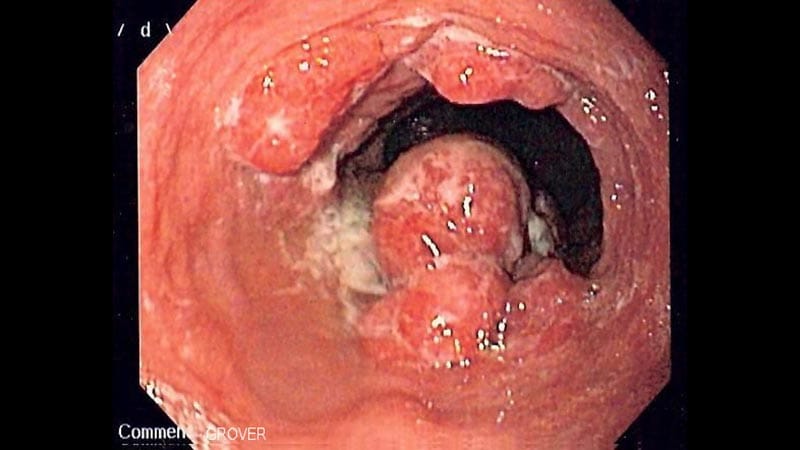
Глибші Запити
How can advancements in biopsy techniques improve the accuracy of preoperative tumor grading
Advancements in biopsy techniques can significantly enhance the accuracy of preoperative tumor grading in several ways. One approach is the utilization of advanced imaging modalities such as confocal laser endomicroscopy or volumetric laser endomicroscopy, which provide real-time, high-resolution images of tissue structures. These techniques allow for better visualization of cellular and subcellular details, aiding in more precise tumor grading.
Moreover, the incorporation of molecular markers and genetic profiling into biopsy analysis can offer additional insights into tumor characteristics beyond traditional histopathology. By identifying specific genetic mutations or biomarkers associated with tumor aggressiveness, clinicians can better predict the tumor grade and tailor treatment strategies accordingly.
Furthermore, the development of liquid biopsy techniques, which involve analyzing circulating tumor cells or cell-free DNA in the blood, can provide a non-invasive method to assess tumor characteristics and monitor treatment response over time. These liquid biopsies can complement traditional tissue biopsies and offer a more comprehensive understanding of the tumor biology.
Overall, by integrating these advanced biopsy techniques into clinical practice, healthcare providers can improve the accuracy of preoperative tumor grading, leading to more personalized and effective treatment decisions for patients with esophageal adenocarcinoma.
Is there a potential for AI or machine learning to enhance the reliability of biopsy results in EAC patients
There is indeed a significant potential for AI and machine learning to enhance the reliability of biopsy results in patients with esophageal adenocarcinoma (EAC). AI algorithms can analyze large volumes of imaging and histopathological data to identify subtle patterns and features that may not be readily apparent to human observers. By training AI models on diverse datasets of biopsy samples and corresponding clinical outcomes, these systems can learn to predict tumor grade with high accuracy.
Machine learning algorithms can also assist in integrating multiple data sources, such as imaging findings, molecular markers, and patient demographics, to generate more comprehensive predictive models for tumor grading. These models can help clinicians make more informed decisions regarding treatment strategies and patient management based on the individual characteristics of each tumor.
Furthermore, AI-powered decision support systems can streamline the interpretation of biopsy results, reducing the potential for human error and variability in grading assessments. By providing clinicians with real-time feedback and recommendations, AI technologies can enhance the reliability and consistency of biopsy interpretations in EAC patients, ultimately improving patient outcomes.
How can the medical community address the challenges of balancing invasive procedures like esophagectomy with less aggressive treatment options based on biopsy results
Addressing the challenges of balancing invasive procedures like esophagectomy with less aggressive treatment options based on biopsy results requires a multidisciplinary approach within the medical community. One key strategy is to establish tumor boards or multidisciplinary teams comprising gastroenterologists, oncologists, radiologists, pathologists, and surgeons to review biopsy findings collaboratively and discuss the most appropriate treatment plan for each patient.
Additionally, the development of clinical practice guidelines and algorithms that outline clear criteria for selecting patients for esophagectomy versus less invasive treatments can help standardize decision-making processes. These guidelines should take into account not only tumor grade but also other factors such as patient comorbidities, performance status, and preferences.
Furthermore, patient education and shared decision-making play a crucial role in determining the most suitable treatment approach based on biopsy results. Clinicians should engage patients in discussions about the risks and benefits of different treatment options, ensuring that individual values and preferences are considered in the decision-making process.
By fostering collaboration among healthcare providers, implementing evidence-based guidelines, and prioritizing patient-centered care, the medical community can effectively navigate the challenges of balancing invasive procedures with less aggressive treatment options in EAC patients, ultimately optimizing outcomes and quality of life for individuals with this condition.
0
