Blood Biomarkers Can Predict Knee Osteoarthritis Development Years Before X-Ray Detection
Core Concepts
A panel of six blood biomarkers can accurately identify individuals at risk of developing radiographic knee osteoarthritis up to 8 years before the disease is detectable on X-rays.
Abstract
The study analyzed blood samples from a population-based, longitudinal study of women in London to identify biomarkers that can predict the development of knee osteoarthritis (OA) before the disease is visible on X-rays. The researchers selected 100 women who went on to develop radiographic knee OA and 100 age- and BMI-matched controls.
Through mass spectrometry and machine learning, the team identified a panel of six peptides corresponding to six proteins that could accurately distinguish women who would develop radiographic knee OA from those who would not, up to 8 years before the X-ray changes were detected. This panel had an area under the receiver operating characteristic curve of 0.77, indicating good predictive performance.
The authors note that this biomarker panel has the potential to identify individuals at risk of developing knee OA in the absence of other clinical risk factors. Previous work has also shown that more than half of the biomarkers that predict incident OA also predict OA progression. The authors suggest that these biomarkers point to an unresolved acute phase response as an underlying disease process.
While the study focused on radiographic OA, the authors acknowledge that clinically relevant OA requires the presence of symptoms like pain and functional impairment, in addition to X-ray changes. Further validation in larger, more diverse cohorts that assess both radiographic and symptomatic OA is needed to fully establish the clinical utility of this biomarker panel.
Blood Biomarkers Predict Knee OA Years in Advance
Stats
The study analyzed blood samples from 100 women who went on to develop radiographic knee OA and 100 age- and BMI-matched controls.
The panel of 6 peptides/proteins could accurately distinguish women who would develop radiographic knee OA from those who would not, up to 8 years before the X-ray changes were detected (area under the receiver operating characteristic curve of 0.77).
More than half (58%) of the biomarkers that predicted incident OA also predicted OA progression in earlier work.
Quotes
"The value of our study is a panel that, in the absence of clinical factors indicative of high-risk knee OA, has the potential to discriminate individuals at risk for incident radiographic knee OA from those not at risk."
"Even for the ones that didn't overlap with OA progression, they all pointed to the same sort of disease process, which is an unresolved acute phase response type of biological process."
Key Insights Distilled From
by Lucy Hicks at www.medscape.com 04-26-2024
https://www.medscape.com/viewarticle/blood-biomarkers-predict-knee-osteoarthritis-years-advance-2024a100085w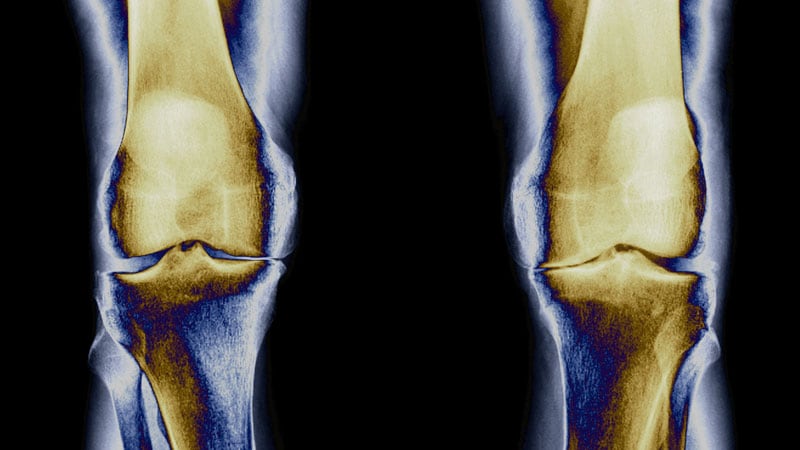
Deeper Inquiries
How can the predictive performance of this biomarker panel be further improved to enhance its clinical utility?
To enhance the predictive performance of the biomarker panel for knee osteoarthritis (OA), several strategies can be considered. Firstly, expanding the study to include a more diverse population, including males and individuals of different ethnic backgrounds, would help validate the findings across a broader demographic. This would ensure that the biomarkers are applicable across various groups and not limited to a specific subset of the population. Additionally, conducting longitudinal studies with larger sample sizes and longer follow-up periods would strengthen the evidence supporting the predictive capabilities of the biomarker panel. Incorporating other types of biomarkers, such as genetic markers or inflammatory markers, could also improve the accuracy of predicting OA development. Furthermore, integrating advanced machine learning algorithms and data analytics techniques could refine the predictive models and increase their sensitivity and specificity. Collaborating with clinicians and researchers in different fields to validate the findings and establish standardized protocols for biomarker testing and interpretation would also be beneficial in enhancing the clinical utility of the biomarker panel.
What are the potential limitations or confounding factors that may affect the accuracy of this approach in predicting clinically relevant knee OA, beyond just radiographic changes?
While the biomarker panel shows promise in predicting the development of knee OA, there are several limitations and confounding factors that could affect its accuracy in predicting clinically relevant knee OA beyond radiographic changes. One key limitation is the focus on radiographic evidence alone, which may not always correlate with symptomatic OA experienced by patients. Factors such as pain, stiffness, and functional impairment are essential components of clinically relevant OA but may not be captured solely through radiographic assessments. Additionally, the study's sample population consisting only of White women may limit the generalizability of the findings to other demographic groups. Other potential confounding factors include comorbidities, lifestyle factors, and genetic predispositions that could influence the development and progression of OA. Moreover, the dynamic nature of OA, with fluctuations in symptoms and disease activity over time, poses a challenge in accurately predicting its course based on static biomarker measurements. Addressing these limitations and considering a more holistic approach that incorporates clinical symptoms, patient-reported outcomes, and other relevant factors would be crucial in improving the accuracy of predicting clinically relevant knee OA.
What other emerging technologies or approaches could be combined with this biomarker panel to provide a more comprehensive assessment of an individual's risk of developing symptomatic and disabling knee OA?
In addition to the biomarker panel, several emerging technologies and approaches could be integrated to offer a more comprehensive assessment of an individual's risk of developing symptomatic and disabling knee OA. One potential approach is the incorporation of imaging modalities beyond traditional X-rays, such as magnetic resonance imaging (MRI) or ultrasound, to evaluate structural changes and soft tissue abnormalities in the joint. Advanced imaging techniques can provide detailed information about cartilage integrity, synovial inflammation, and subchondral bone alterations, complementing the information obtained from blood biomarkers. Furthermore, wearable sensors and digital health tools could be utilized to monitor biomechanical factors, gait patterns, and physical activity levels, which are known to influence OA progression. By combining data from multiple sources, including biomarkers, imaging, and digital health monitoring, a more personalized and dynamic risk assessment model could be developed. Integrating artificial intelligence (AI) algorithms for data analysis and predictive modeling could also enhance the accuracy and predictive power of the combined approach. Collaborating with interdisciplinary teams comprising orthopedic specialists, rheumatologists, data scientists, and engineers would facilitate the integration of these technologies and approaches to provide a holistic evaluation of an individual's risk of developing symptomatic and disabling knee OA.
0
