Gut Microbiome Signatures Linked to KRAS Mutations in Colorectal Cancer Patients
Core Concepts
Gut microbiota signatures can serve as noninvasive biomarkers to identify KRAS mutation status in colorectal cancer patients and guide personalized treatment.
Abstract
Researchers have identified distinct gut microbiota signatures associated with KRAS mutations in colorectal cancer (CRC) patients. The study found that:
At the genus level, Fusobacterium, Clostridium, and Shewanella were more abundant in the KRAS mutant group, while Bifidobacterium and Akkermansia were more abundant in the KRAS wild-type group.
The isoflavonoid biosynthesis pathway was significantly higher in the KRAS wild-type group compared to the KRAS mutant group, suggesting it may inhibit CRC development and progression.
The researchers developed a machine learning model that can predict KRAS mutation status in CRC patients based on the gut microbiota signature, with potential for clinical application.
These findings contribute to the understanding of the interplay between gut dysbiosis and KRAS mutations in CRC pathogenesis, and highlight the potential of gut microbiota as noninvasive biomarkers to guide personalized CRC treatment.
Microbial Signature of KRAS-Mutated CRC Identified
Stats
About 40% of people with colorectal cancer have a KRAS mutation.
The researchers analyzed stool samples from 94 CRC patients, including 24 with KRAS-mutated CRC and 70 with KRAS wild-type CRC.
Quotes
"Our new work contributes to the growing body of evidence highlighting the significance of microbiota-driven mechanisms in cancer pathogenesis."
"It is postulated that KRAS wild-type CRC may be less aggressive due to the upregulation of the isoflavonoid biosynthesis pathway, which may inhibit CRC development and progression."
Key Insights Distilled From
by Megan Brooks at www.medscape.com 04-17-2024
https://www.medscape.com/viewarticle/microbial-signature-kras-mutated-colorectal-cancer-2024a10007en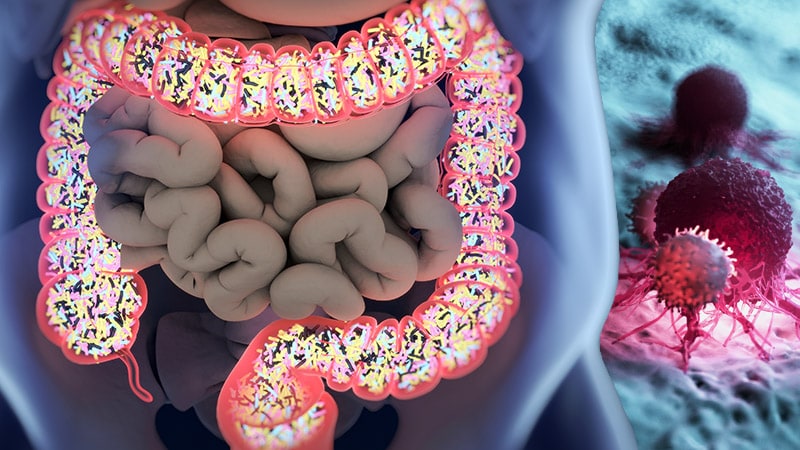
Deeper Inquiries
How can the gut microbiome-based predictive model be further improved and validated for clinical use?
To further enhance and validate the gut microbiome-based predictive model for clinical use, several steps can be taken. Firstly, expanding the cohort size to include a larger and more diverse group of CRC patients can help improve the model's accuracy and reliability. This larger dataset would provide more robust data for analysis and validation. Additionally, longitudinal studies tracking changes in the gut microbiome over time in relation to KRAS mutation status and CRC progression can offer valuable insights into the dynamic nature of these interactions.
Furthermore, incorporating multi-omics approaches, such as metagenomics, metabolomics, and transcriptomics, can provide a more comprehensive understanding of the molecular mechanisms underlying the relationship between gut microbiota and KRAS mutations in CRC. Integrating these diverse data types can help identify key biomarkers and pathways that influence CRC development and treatment response.
Validation of the predictive model can be done through independent cohorts to assess its generalizability and reproducibility across different patient populations. External validation in real-world clinical settings can further confirm the model's utility and effectiveness in predicting KRAS mutation status in CRC patients. Continuous refinement and optimization of the model based on feedback from clinical applications and new research findings will be essential to ensure its accuracy and clinical relevance.
What are the potential mechanisms by which the identified gut microbiota taxa influence KRAS mutation status and CRC progression?
The identified gut microbiota taxa, such as Fusobacterium, Clostridium, and Shewanella, can influence KRAS mutation status and CRC progression through various mechanisms. Fusobacterium, for instance, has been linked to CRC development and is associated with KRAS mutations. It can promote inflammation, alter the immune response, and induce DNA damage, all of which can contribute to tumor initiation and progression in KRAS-mutated CRC.
Clostridium, known for producing metabolites that can cause DNA damage and trigger inflammatory responses, may create a microenvironment conducive to tumor growth and progression in KRAS-mutated CRC. Similarly, Shewanella has been implicated in CRC development and may play a role in promoting tumor growth and metastasis in the presence of KRAS mutations.
On the other hand, gut microbiota taxa like Bifidobacterium and Akkermansia, which were abundant in the KRAS wild-type group, may exert protective effects against CRC development. Bifidobacterium, with its antitumor activity, and Akkermansia, a potential probiotic, could help maintain gut homeostasis, modulate the immune response, and inhibit tumor growth, thereby reducing the likelihood of KRAS mutation and CRC progression.
Overall, these gut microbiota taxa can influence KRAS mutation status and CRC progression through their effects on inflammation, immune modulation, metabolite production, and tumor microenvironment, highlighting the intricate interplay between the gut microbiome and colorectal cancer pathogenesis.
What other molecular or genetic factors interact with the gut microbiome to shape CRC development and treatment response?
In addition to KRAS mutations, several other molecular and genetic factors interact with the gut microbiome to shape CRC development and treatment response. For example, mutations in other oncogenes such as APC, TP53, and BRAF can influence the composition and function of the gut microbiota, leading to alterations in tumor growth, metastasis, and treatment outcomes. These genetic alterations can create a microenvironment that favors the growth of specific microbial taxa associated with CRC progression.
Moreover, host genetic factors, including variations in immune response genes, mucin production, and epithelial barrier integrity, can modulate the interaction between the gut microbiome and CRC development. Genetic polymorphisms that affect the host-microbiota crosstalk may impact inflammatory pathways, immune surveillance, and tumor microenvironment, ultimately influencing the risk of CRC and response to therapy.
Furthermore, epigenetic modifications, such as DNA methylation and histone acetylation, can regulate gene expression in both the host and the gut microbiota, shaping their interactions and impacting CRC pathogenesis. These epigenetic changes can alter the microbial composition, immune response, and metabolic pathways in the gut, contributing to CRC development and treatment resistance.
Understanding the complex interplay between molecular and genetic factors, along with the gut microbiome, is crucial for unraveling the mechanisms underlying CRC pathogenesis and for developing personalized therapeutic strategies that target both the tumor and its microenvironment.
0
