Risk-Adapted Neoadjuvant Chemoradiotherapy in Rectal Cancer Study Findings
Основные понятия
Tailoring neoadjuvant therapy in rectal cancer based on risk classification improves outcomes.
Аннотация
TOPLINE:
- Low-risk rectal cancer patients may avoid neoadjuvant chemoradiotherapy (nCRT) with low local relapse risk.
METHODOLOGY:
- Study classified cT2-4 rectal cancer patients into high and low-risk groups.
- 530 low-risk patients had upfront total mesorectal excision (TME), while 354 high-risk patients received nCRT then TME.
- Primary endpoint: 5-year locoregional recurrence; secondary: 5-year distant metastases.
- Subgroup analysis: 570 patients with lower/middle rectal third tumors, clinical stages II/III, divided into risk groups.
TAKEAWAY:
- 5-year locoregional recurrence: 4.1% for protocol-treated, 2.9% for low-risk upfront TME, 5.7% for high-risk nCRT+TME.
- 5-year distant metastases: 15.9% low-risk, 30.5% high-risk.
- Subgroup: low-risk had 3.8% locoregional recurrence, 16.8% distant metastases.
- High-risk subgroup with nCRT+TME had 34.5% metastases risk.
IN PRACTICE:
- Support for de-escalation in low-risk and escalation in high-risk patients for better outcomes.
STUDY DETAILS:
- Led by Reinhard Ruppert, MD, published in the Journal of Clinical Oncology.
LIMITATIONS:
- Nonrandomized study, lacked true comparator group, high protocol deviation.
DISCLOSURES:
- No commercial funding, Ruppert had no relevant disclosures, some authors had relationships with various companies.
Настроить сводку
Переписать с помощью ИИ
Создать цитаты
Перевести источник
На другой язык
Создать интеллект-карту
из исходного контента
Перейти к источнику
www.medscape.com
Risk-Adapted Neoadjuvant Chemoradiotherapy in Rectal Cancer?
Статистика
The overall 5-year locoregional recurrence was 4.1% for protocol-treated patients, 2.9% for low-risk patients who had upfront TME, and 5.7% for high-risk patients who had nCRT followed by TME.
The 5-year rates of distant metastases were 15.9% for low-risk patients and 30.5% for high-risk patients.
In the subgroup, low-risk patients had slightly higher rates of 5-year locoregional recurrence (3.8%) and distant metastases (16.8%).
In the subgroup, high-risk patients with involved mesorectal facia and/or cT4 tumors who received nCRT then TME exhibited the highest risk of metastases (34.5%).
Цитаты
"These data support de-escalation of nCRT in low-risk patients and escalation of neoadjuvant therapy in high-risk patients to improve long-term outcomes."
Ключевые выводы из
by Megan Brooks в www.medscape.com 06-27-2023
https://www.medscape.com/viewarticle/993763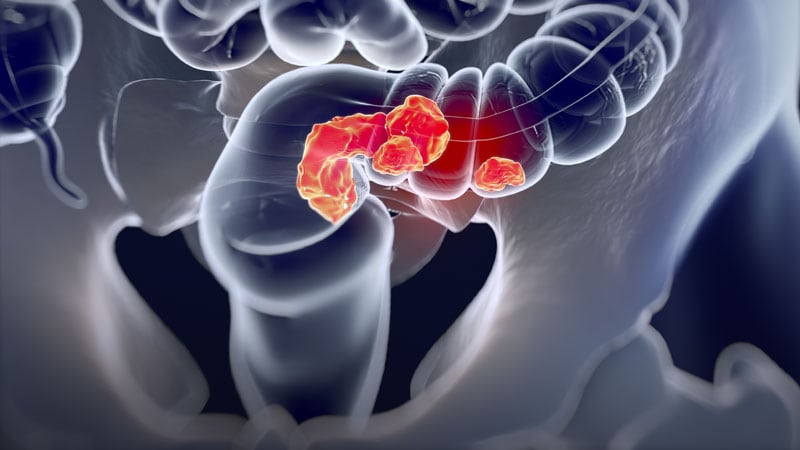
Дополнительные вопросы
How can risk-adapted neoadjuvant therapy be implemented effectively in clinical practice
Implementing risk-adapted neoadjuvant therapy effectively in clinical practice requires a multidisciplinary approach. Firstly, accurate risk stratification based on a combination of clinical, radiological, and pathological factors is crucial. This involves identifying low-risk patients who may safely skip neoadjuvant chemoradiotherapy (nCRT) and proceed directly to surgery, as well as high-risk patients who would benefit from intensified neoadjuvant treatment.
Secondly, clear treatment algorithms and guidelines need to be established to guide clinicians in decision-making. These protocols should outline the criteria for risk stratification, the recommended treatment approach for each risk group, and the monitoring of treatment response. Regular multidisciplinary tumor boards can aid in discussing complex cases and ensuring adherence to the risk-adapted approach.
Furthermore, patient education and shared decision-making are essential components of implementing risk-adapted therapy. Patients should be informed about the rationale behind the treatment recommendations, the potential benefits and risks, and the importance of adherence to the personalized treatment plan. Engaging patients in the decision-making process can improve treatment compliance and outcomes.
Continuous evaluation and quality assurance are also necessary to monitor the effectiveness of risk-adapted therapy in clinical practice. Regular audits, outcome assessments, and feedback mechanisms can help identify areas for improvement and optimize patient care. By integrating these elements, healthcare providers can effectively implement risk-adapted neoadjuvant therapy and improve outcomes for patients with rectal cancer.
What are the potential implications of the high protocol deviation in the study results
The high protocol deviation observed in the study results has several potential implications that may impact the interpretation and generalizability of the findings. Firstly, protocol deviations can introduce bias and confound the results, leading to inaccurate conclusions about the effectiveness of risk-adapted neoadjuvant therapy. In this study, the nonrandomized design and lack of a true comparator group already pose limitations, and high protocol deviation further complicates the interpretation of the data.
Moreover, high protocol deviation may indicate challenges in implementing risk-adapted therapy in real-world clinical settings. It suggests variability in treatment decisions, adherence to protocols, and patient management practices among different healthcare providers. Understanding the reasons behind protocol deviations, such as clinician preferences, patient factors, or institutional practices, is crucial for addressing these challenges and improving the consistency of care delivery.
Additionally, high protocol deviation can impact the reproducibility and external validity of the study results. Replicating the findings in other settings or populations may be challenging if there is significant variability in how the treatment protocol is implemented. Therefore, efforts to minimize protocol deviations, standardize treatment protocols, and enhance adherence to guidelines are essential for ensuring the reliability and applicability of research findings in clinical practice.
How might the findings of this study impact the future of personalized cancer treatment strategies
The findings of this study have significant implications for the future of personalized cancer treatment strategies, particularly in the context of rectal cancer management. By demonstrating the feasibility and efficacy of risk-adapted neoadjuvant therapy, the study supports a more tailored and individualized approach to treatment decision-making. This shift towards personalized medicine in oncology can lead to improved outcomes, reduced treatment-related toxicities, and enhanced patient satisfaction.
The identification of low-risk patients who can safely avoid neoadjuvant chemoradiotherapy (nCRT) and proceed directly to surgery highlights the importance of avoiding overtreatment and minimizing unnecessary interventions. This approach not only spares patients from potential side effects of nCRT but also streamlines the treatment pathway, potentially reducing healthcare costs and resource utilization.
Conversely, the recognition of high-risk patients who may benefit from intensified neoadjuvant therapy underscores the need for precision medicine in oncology. Tailoring treatment strategies based on individual risk profiles, tumor characteristics, and treatment responses can optimize outcomes and survival rates for patients with aggressive or advanced disease.
Overall, the findings of this study support the paradigm shift towards personalized cancer care, emphasizing the importance of risk stratification, treatment individualization, and multidisciplinary collaboration in improving the management of rectal cancer and potentially other malignancies. This approach holds promise for enhancing treatment outcomes, quality of life, and long-term survival for cancer patients.
0
